Careful preoperative evaluation prior to cataract surgery is integral to delivering improved refractive outcomes. Corneal topography, in particular, has become an invaluable tool in preoperative planning. With this in mind, we present the following case report.
A 62-year-old man presented for cataract evaluation in his right eye. Preoperative corneal topography identified mild inferior steepening in each eye (Figure 1). Cataract surgery was performed in the patient’s right eye with an excellent postoperative course.
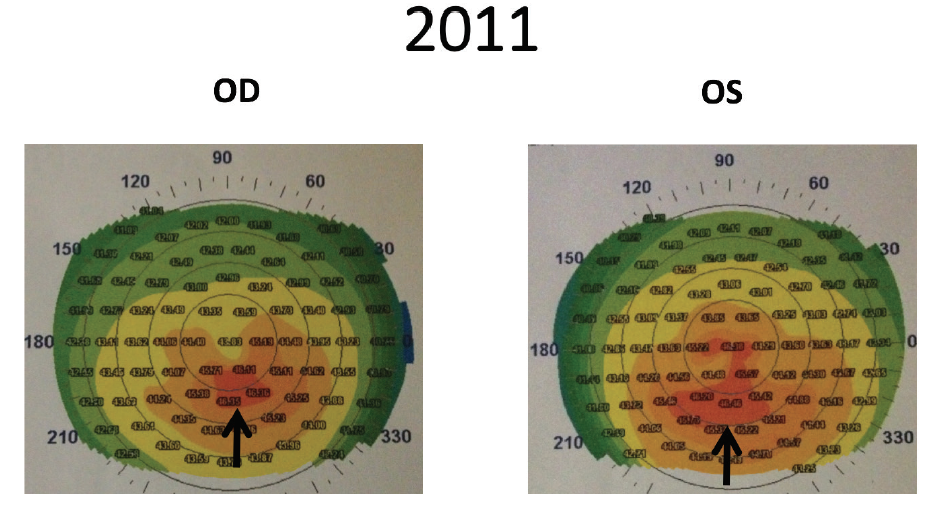
Figure 1. Corneal topography in 2011 demonstrated mild inferior steepening (black arrows), greater in the patient’s left eye than in the right.
Two years later, the patient returned with a visually significant cataract in his left eye. Corneal topography was repeated (Figure 2). At that time, the inferior-superior (I-S) ratio—a metric used to evaluate the severity of keratoconus—was measured at 2.67. This confirmed progressive inferior steepening in the left eye when compared to the initial topography from 2 years before, when an I-S ratio of 2.24 (Figure 2) was measured. Furthermore, repeat biometry showed a 1.50 D reduction in the preferred IOL power, from 19.50 to 18.00 D, due to an increase in corneal power over the 2 years since his first cataract surgery procedure (Figure 3).
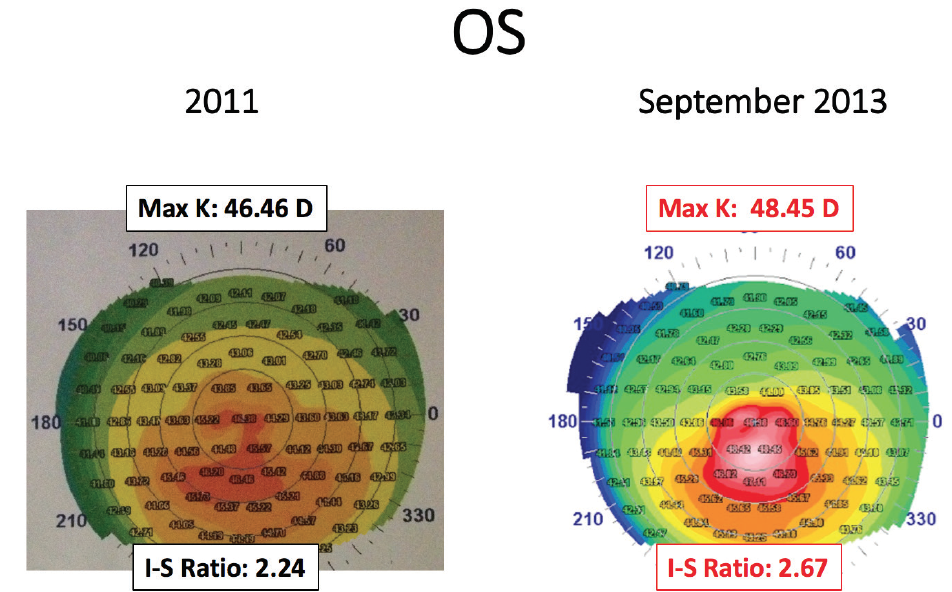
Figure 2. A comparison of corneal topographies in the patient’s left eye showed progressive inferior steepening with an increased I-S ratio over a period of 2 years, suggesting keratoconus.
Figure 3. Biometry in the patient’s left eye showed a significant change in keratometry between 2011 and 2013 that contributed to a 1.50 D reduction in IOL power.
At this juncture, the differential diagnoses of unilateral irregular astigmatism were considered. These differentials included ocular surface disease (OSD), epithelial basement membrane dystrophy (EBMD), development of a Salzmann nodule, corneal scarring, and keratoconus. The patient’s history was negative for most of the aforementioned diagnoses, and the anterior and posterior segment examinations were entirely normal, with the exception of decreased tear breakup time and trace inferior punctate epithelial erosions, consistent with OSD.
The diagnosis of progressive unilateral keratoconus was entertained, given the worsening inferior steepening and significant I-S ratio demonstrated on topography. Although progressive keratoconus is uncommon in patients in their 60s, keratoconus itself occurs with relative frequency. Risk factors for progressive keratoconus include vigorous eye rubbing and a significant family history; however, this patient attested to neither of these.
After treatment for OSD, the patient successfully underwent cataract surgery in his left eye with implantation of a monofocal IOL. The choice of IOL power was decreased by 1.50 D compared with IOL calculations from 2 years prior, in order to compensate for the increased corneal curvature and to attain the patient’s desired postoperative outcome of slight myopia to emmetropia. The lens power choice highlights the importance of repeating biometry if there exists any doubt as to the accuracy of initial measurements or if there was an extended period between measurement and surgery, as was the case here.
It is of note that the choice of a monofocal IOL was made given the irregular astigmatism in that eye and the concern for the possibility of other underlying corneal pathology. Placing a multifocal IOL in such cases increases the risk of decreased patient satisfaction and reduced quality of vision.
The patient’s BCVA immediately after cataract extraction was 20/25 OS. Two months later, the patient returned complaining of worsening blurry vision OS with BCVA of 20/30. Anterior and posterior segment exams appeared normal; however, following instillation of fluorescein dye, the patient demonstrated a small area of negative staining inferiorly (Figure 4), which had not been evident preoperatively.
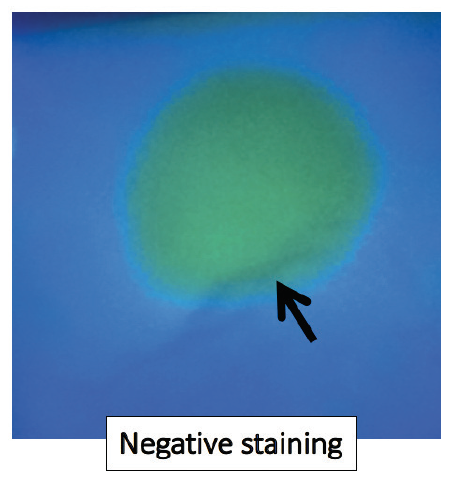
Figure 4. Slit-lamp examination of the cornea with fluorescein dye revealed an inferior epithelial ridge with negative staining (black arrow) suggestive of EBMD.
The area of negative staining was consistent with a diagnosis of map-dot-fingerprint dystrophy or EBMD. Coincidentally, the area of EBMD observed on slit-lamp examination corresponded to the worsening inferior steepening demonstrated on corneal topography. A diagnosis of EBMD masquerading as a late-onset unilateral keratoconus was made. Because the slit-lamp examination of the fellow eye was entirely within normal limits, without evidence of EBMD, we also considered that the findings in the patient’s left eye might simply represent localized epithelial hyperplasia.
EBMD IDENTIFICATION AND TREATMENT OPTIONS
EBMD is present in 6% to 18% of the population, predominantly in women older than 50 years of age.1 The typical presentation may include blurry vision, monocular diplopia, ghost images, and recurrent corneal erosions. There have also been case reports of EBMD masquerading as keratoconus. In a retrospective review of 1,000 cases of presumed corneal ectasia (keratoconus, keratoglobus, pellucid marginal degeneration) referred for possible CXL, PRK, or intrastromal corneal ring segment placement, 26 eyes of 20 patients had been falsely diagnosed with an ectatic disorder.2 Of the misdiagnosed cases, the true underlying pathology in nine eyes was EBMD. Other etiologies included superficial punctate keratitis (n = 7), high astigmatism (n = 3), amiodarone keratopathy (n = 2), corneal warping (n = 2), corneal scars (n = 1), and measurement error (n = 2). In another study, Reinstein et al found utility in epithelial thickness profiling with VHF ultrasound to confirm nonkeratoconic pathology in eyes that would normally have been classified as keratoconic based on corneal topography.3
Treatment of EBMD is not necessary if a patient is asymptomatic; however, lubricants, hypertonic solutions, and contact lenses may be trialed as initial conservative management. Surgical treatments for visually significant EBMD include simple epithelial debridement, with or without diamond burr polishing, and phototherapeutic keratectomy (PTK).
In a study by Itty et al, 74 eyes of 55 patients underwent simple mechanical debridement, resulting in average BCVA improvement from 20/44 to 20/33.4 In that study, EBMD recurred in 18 of the 74 eyes. No infections or persistent epithelial defects were reported, but subepithelial haze was present in 19 eyes.
Lee et al sought to examine the efficacy of PTK in the management of EBMD.5 After PTK, 58 eyes of 51 patients who had not responded to conservative management for EBMD experienced an average BCVA improvement from 20/32 to 20/25. In 29 eyes with recurrent erosions, the average BCVA improvement was from 20/25 to 20/20. These authors concluded that PTK was safe and effective over the long term with results comparable to those of other surgical modalities.
WHAT WE DID
After discussing the options, the patient decided to undergo PTK in his left eye. Following the procedure, the topography normalized (Figure 5) and BCVA improved to 20/20. The keratometry in that eye returned to the value seen in the original biometry readings performed at the time of his initial presentation 26 months earlier. The flattened keratometry resulted in a hyperopic shift to +1.50 +1.00 x 180°. Although the patient’s BCVA was 20/20, he desired to be spectacle-free, and he therefore underwent a piggyback IOL procedure to improve his distance vision.
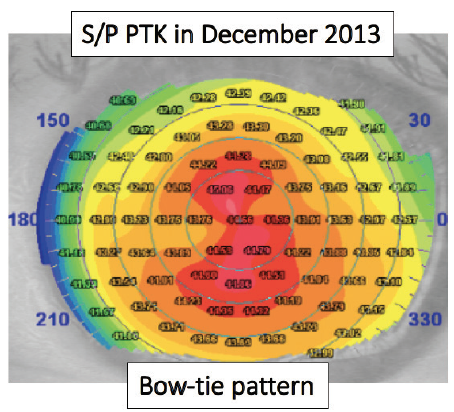
Figure 5. Topography of the patient’s left eye from January 2014 after PTK in December 2013 demonstrates the bow-tie pattern of regular astigmatism.
This case brings to light a unique manner in which EBMD may present, as well as the medical and surgical implications of this presentation. Specifically, the case demonstrates the importance of a thorough slit-lamp examination with the use of fluorescein dye, repeated pre- and postoperative testing to ensure accurate assessments of keratometry, and implantation of monofocal IOLs in eyes in which other underlying corneal pathology might be present.
1. Weisenthal RW. External Disease and Cornea. In: Basic and Clinical Science Course. San Francisco: American Academy of Ophthalmology; 2017.
2. Stein R, Salim G. False corneal ectasia in patients referred for corneal crosslinking, topography-guided photorefractive keratectomy, and intrastromal corneal rings. Can J Ophthalmol. 2019;54(3):374-381.
3. Reinstein DZ, Archer TJ, Gobbe M. Stability of LASIK in topographically suspect keratoconus confirmed non-keratoconic by Artemis VHF digital ultrasound epithelial thickness mapping: 1-year follow-up. J Refract Surg. 2009;25(7):569-577.
4. Itty S, Hamilton SS, Baratz KH, Diehl NN, Maguire LJ. Outcomes of epithelial debridement for anterior basement membrane dystrophy. Am J Ophthalmol. 2007;144(2):217-221.
5. Lee WS, Lam CK, Manche EE. Phototherapeutic keratectomy for epithelial basement membrane dystrophy. Clin Ophthalmol. 2017;11:15-22.