

It is only in the past 15 years that we have really started focusing on the importance of astigmatism management during cataract surgery. Our journey with toric IOLs started around 2005. In a study of more than 2,000 of our own patients undergoing cataract surgery, we found that more than 50% had at least 0.50 D of preexisting corneal astigmatism and a large proportion of these had more than 1.00 D of astigmatism (unpublished data). We also calculated our surgically induced astigmatism, and we realized that, if we incorporated this figure into preexisting astigmatism, a large majority of patients now had treatable degrees of astigmatism.
As our efforts have led to improvements in the spherical refractive outcomes of cataract surgery, it is now time that we address this important entity, astigmatism. Studies have shown that greater than 0.50 D of astigmatism can degrade visual performance, including reading speed and contrast sensitivity.1 In earlier days, we treated corneal astigmatism only when it exceeded 1.00 D, but today, with better precision technology, any amount of astigmatism is potentially correctable.
We have never been big proponents of incisional astigmatic correction, whether manual or laser-assisted. The major reasons have been the variability of outcomes from eye to eye, the regression of correction over time, and the induction of ocular surface disturbances. For these and other reasons, we favor toric IOL implantation to correct existing astigmatism
THE NITTY GRITTY
The nitty gritty of toric IOL implantation is not very different or more difficult than sphere-only IOL surgery, except that a few additional steps are required perioperatively. For every eye, a cataract preoperative examination begins with an assessment of corneal astigmatism before instillation of any medications.
We prefer to use a combination of manual keratometry, automated keratometry (Lenstar, Haag-Streit), and corneal tomography including posterior corneal assessment (Pentacam, Oculus Optikgeräte) to document magnitude, direction, and regularity of corneal astigmatism. Optical biometry is performed, and we also routinely perform ray-tracing aberrometry and retinal OCT for all patients. These measurements help us to detect potential sources of postoperative visual dissatisfaction and to counsel patients accordingly.
For IOL power calculation, we recently switched to the Barrett Universal II formula and the Barrett Toric Calculator for all toric IOL implantations, and we find that these work well.
MARKING THE CORNEA
One area that has always been a challenge in toric IOL practice is the methodology for marking the cornea. Having tried various ways of marking the cornea preoperatively, we settled in the past for manual, freehand marking. Recently, since our acquisition of the digital Verion Image Guided System (Alcon) for IOL planning and implantation, we rely on this system.
Our outcomes have greatly improved with the combination of all these technologies, and we now feel confident in suggesting toric IOLs to anyone who has treatable, regular corneal astigmatism. This includes challenging situations, such as patients with small pupils and selected eyes with zonular weakness.
Toric IOLs are also useful in cataract surgery for children less than 5 years old. In this age group, when amblyopia is a threat, correcting astigmatism and giving the child the best possible unaided quality of vision is a huge help in combating any initial amblyopia (Figure).
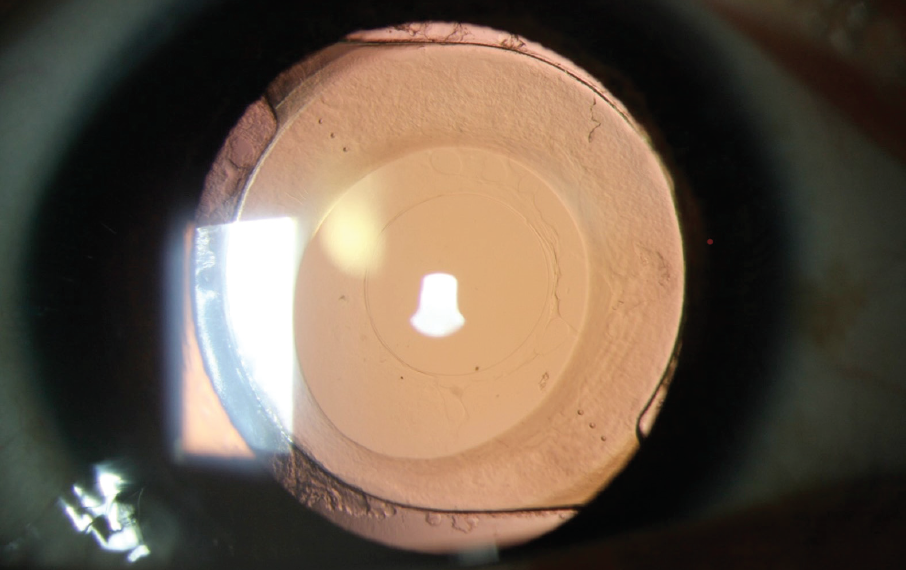
Figure. Postoperative slit-lamp image of a pediatric eye that underwent anterior and posterior capsulorhexis and toric IOL implantation.
CONCLUSION
We strongly believe that astigmatism greater than 0.50 D must be addressed in this modern era, especially with patients now demanding excellent unaided visual quality and presbyopia correction. The biggest clincher in decision-making for IOL selection, we believe, is the presence or absence of corneal astigmatism. Further, the best thing about toric IOLs is that there are practically no downsides, such as dysphotopsia. And even if you end up with a refractive surprise, there are options to correct it.
Now, with the ability to correct lower amounts of astigmatism with the broad range of toric IOL powers available, about 50% of our toric practice is in patients with low amounts of astigmatism (<1.50 D). If we stick to a set regimen in our preoperative evaluations and ensure precision in all our measurements, we believe toric IOLs can add a wow factor in each surgeon’s practice.
Find out how we address residual postoperative astigmatism in the Table. Click here!
1. Lehmann R, Houtman D. Visual performance in cataract patients with low levels of postoperative astigmatism: full correction versus spherical equivalent correction. Clinical Ophthalmology. 2012:6;333-338.




