CASE PRESENTATION
A 32-year-old woman presents for a routine LASIK consultation. The patient typically wears daily disposable soft contact lenses.
Upon examination, her distance UCVA is 6/60 (20/200) OU. Her BCVA is 20/16 OD and 20/20-2 OS. She accepts a refraction of -5.00 -1.00 x 180º OD and -6.00 -0.50 x 10º OS. The ocular examination is unremarkable except for some mild meibomian gland dysfunction (MGD). Corneal tomography (Figures 1 and 2) and OCT epithelial thickness mapping (Figure 3) are performed.
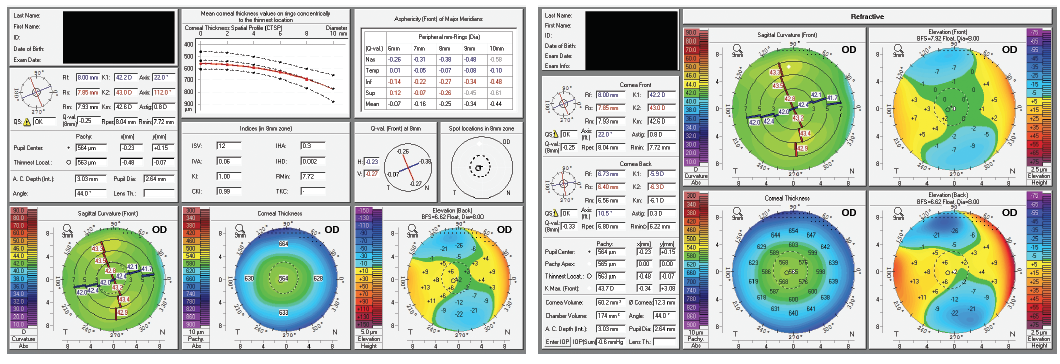
Figure 1. Elevation-based corneal tomography of the patient’s right eye.
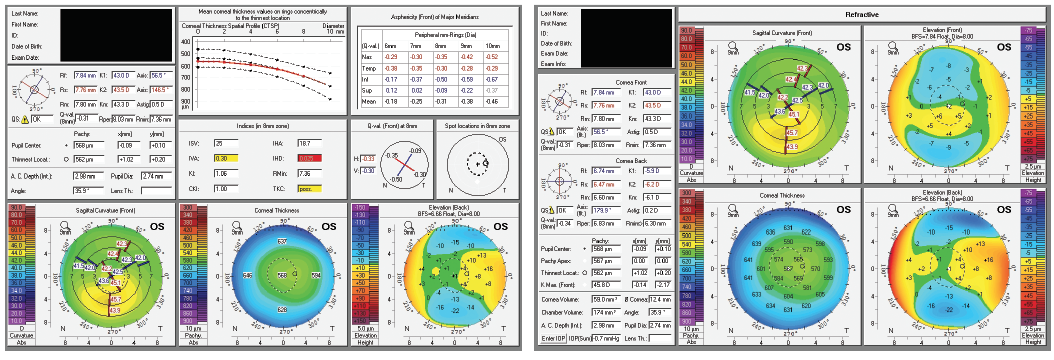
Figure 2. Elevation-based corneal tomography of the patient’s left eye.
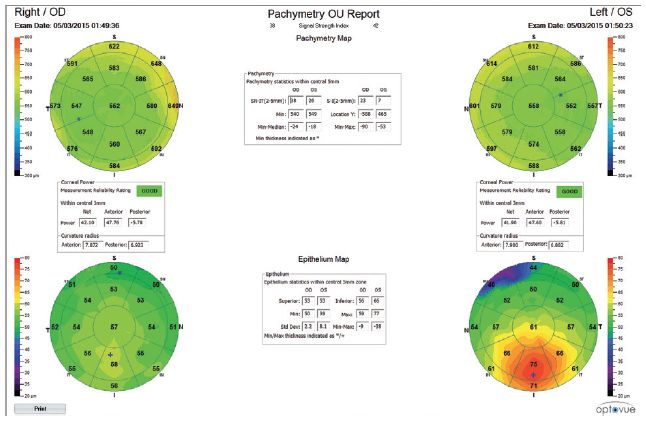
Figure 3. OCT epithelial thickness maps.
How would you proceed?
—Case prepared by Allon Barsam, MA, MBBS, FRCOphth

Arthur B. Cummings, MB CHB, FCS(SA), MMED(OPHTH), FRCS(EDIN)
With elective surgery, the key issue is safety, so I would proceed only if I were convinced that all preoperative findings supported an excellent expected outcome. This patient’s right eye meets all of the preoperative requirements to support an excellent outcome using LASIK, PRK, or a Visian ICL (STAAR Surgical).
Her left eye is trickier. There is inferior steepening of the anterior surface. The tomographic keratoconus indices suggest that keratoconus is a possibility. The epithelial maps suggest a different potential cause for the inferior steepening, however. The maps show thickening of the epithelium inferiorly, but one would expect thinning of the epithelium in keratoconus. Inferior steepening could be caused by contact lens warpage or eye rubbing that has not yet caused stromal thinning. Even sleeping on the stomach or the left side and sleeping on the hands can cause warpage. Finally, MGD and the suboptimal ocular surface could also have affected the scans.
I would ask the patient to stop wearing contact lenses; to optimize the tear film by means of warm compresses, for example; and to be aware of eye rubbing and her sleeping position. I would then repeat the scans in 4 weeks’ time. If they looked the same, although I think LASIK would be a safe option, I would recommend PRK or implantation of a Visian ICL instead. If the tomography and epithelial maps improved, then I believe that LASIK would be safe but perhaps not the best option.
In short, I believe that this patient is not at increased risk of post-LASIK ectasia and that LASIK would be a safe option, but I would recommend transepithelial PRK (Streamlight on the WaveLight EX500 platform, Alcon). In my experience, this procedure achieves excellent refractive outcomes, is safer than LASIK from a corneal biomechanical standpoint, and provides an opportunity to regularize the underlying stroma.

ERIC D. DONNENFELD, MD
This case represents a multitude of possibilities as to the etiology of the corneal steepening in the patient’s left eye. The initial concern is that tomography suggests forme fruste keratoconus, so the patient should be treated accordingly. Her visual acuity is mildly reduced at 20/20- in the left eye compared to 20/16 in the right eye, and the inferior steepening is an issue. Other findings, however, suggest that this is not forme fruste keratoconus. The pachymetry maps show a thick central cornea, and the thinnest area is at the apex of the cornea, which is to be expected in a healthy eye. There would be decentration of the thinnest region inferotemporally or at the apex of the cone if this were keratoconus. Additionally, pachymetry shows thickening of the cornea over the cone, which is the opposite of what would be expected in keratoconus. The epithelial thickness map reveals markedly thick epithelium over the steep area, which again is the opposite of what would be seen in keratoconus and suggests that the etiology of the inferior steepening is simply corneal remodeling, possibly from contact lens wear or MGD in this case. Basement membrane dystrophy and Salzman nodules could have a similar appearance.
I would treat this patient with aggressive ocular surface management, including hot compresses, lid hygiene, oral omega-3 fatty acid fish oil, and topical corticosteroids. Most important, I would have her discontinue contact lens wear and ask her to return for another evaluation in 1 month. If topography or tomography had improved at that time but was not perfect, I would instruct the patient to stay out of contact lenses and bring her back again 1 month later. If the cornea had not changed at that point, I would consider performing epithelial debridement and allowing new epithelium to remodel the cornea over a period of 2 to 3 months before performing laser vision correction.

WHAT I DID: ALLON BARSAM, MA, MBBS, FRCOPHTH
After a conservative period of 2 months with reduced contact lens wear (complete cessation for 3 weeks) and ocular surface management, the patient’s topographic and epithelial status remained unchanged. I therefore carried out an alcohol debridement of the epithelium and 5-µm phototherapeutic keratectomy on the left eye only. Two months later, the topography and epithelial thickness had normalized, and the refraction had changed slightly. Once the refraction in the left eye stabilized, I performed uncomplicated bilateral LASIK. Three months after surgery, the patient’s UCVA was 20/12 OU.




