Limbal relaxing incisions (LRIs), whether performed as standalone procedures or during cataract surgery, provide the surgeon with a tool to improve patients’ quality of vision, quality of life, and satisfaction with their cataract surgery. LRIs and their cousins, astigmatic keratotomies (AKs), require careful management and execution.
PROS AND CONS
To define our terms at the outset, LRIs are partial-thickness corneal incisions placed adjacent to the limbus along the steep meridian. Arcuate AKs are similar incisional procedures, performed more centrally toward the visual axis. Useful for correction of 3.00 D or less of regular corneal astigmatism, LRIs reduce astigmatism by relaxing the steep axis of the cornea while simultaneously steepening the flat axis in a 1:1 ratio, a phenomenon known as coupling.
The advantages of LRIs over AKs include relative ease of performance, less tendency to cause axis shift, less resulting irregular astigmatism, less dependence on pachymetry, less likelihood of overcorrection, smoother postoperative topography, and faster postoperative stabilization of refraction. AKs, on the other hand, have the advantage of being shorter, more powerful incisions.
Relative contraindications to AKs and LRIs include previous radial keratotomy, keratoconus, other topographic abnormalities including irregular astigmatism, and known peripheral corneal disease. LRIs tend to work well for low to moderate amounts of astigmatism (< 3.00 D) and very well for 0.50 D of cylinder up to 1.50 D. For patients with more than 1.50 D of astigmatism, one should take into account increased risks for residual irregular astigmatism and dry eye. For these patients, a toric IOL or excimer laser photoablation may be a better choice to address their astigmatism.
NOMOGRAMS
Several nomograms have been proposed for determining AK and LRI positioning and length. Most nomograms are adjusted for age, sex, and cylinder axis, making them detailed and complex, and this may give the impression that these procedures are extremely precise and unforgiving. In my opinion, however, this simply is not the case. Placement of astigmatic incisions, especially manual ones, remains as much an art as it is a science.
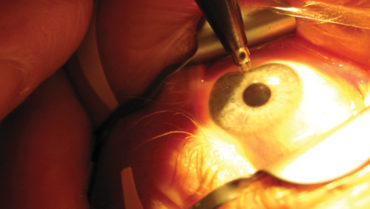
For novice surgeons, a simple nomogram may be favored, such as the Donnenfeld nomogram, which works extremely well for this purpose (Figure 1). The online calculator employs vector analysis to calculate incision parameters based on preoperative patient keratometry, surgically induced astigmatism, and the location of a planned primary cataract incision. If the Donnenfeld or Nichamin nomogram is used, a visual map showing the axis and lengths of incisions will be provided, and a printout of the LRI calculator can be brought to the OR and used as a guide when marking the cornea and performing the LRIs. In general, it is best for surgeons to practice the techniques of LRIs and develop their own nomogram to achieve consistent results.
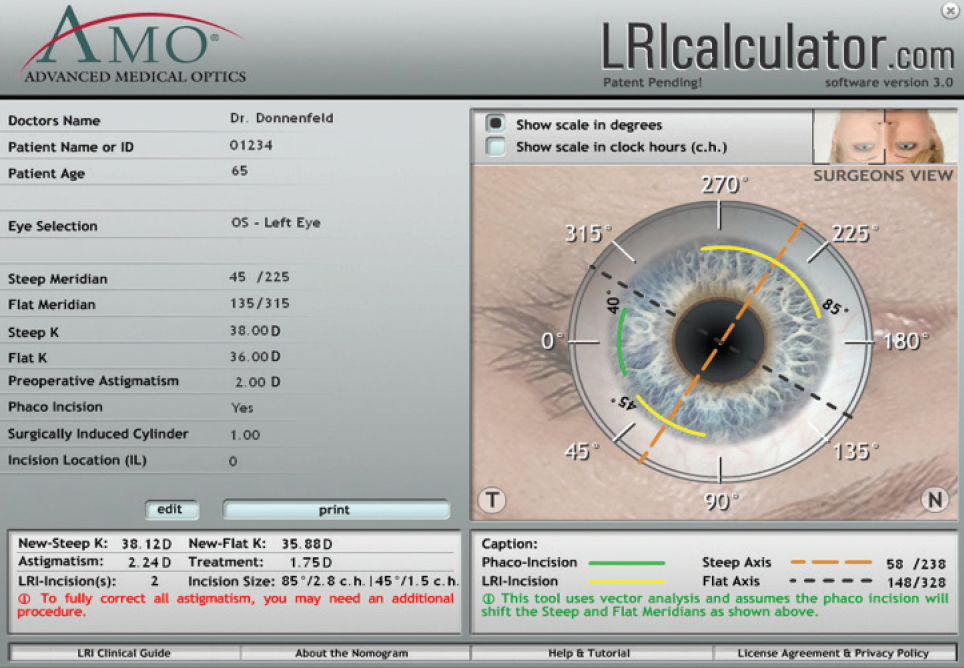
Figure 1. The Donnenfeld nomogram (LRIcalculator.com).
STEP BY STEP
The OR is the best place to start performing astigmatic incisions, which are often combined with routine cataract surgery. When cataract surgery is planned, it is important to account for astigmatism, whether preexisting or surgically induced.
Residual astigmatism of 0.50 D or even less can result in glare, symptomatic blur, ghosting, and halos. The reduced quality of vision associated with residual astigmatism after cataract surgery is magnified in patients with multifocal IOLs. As a result, in recent years, increased emphasis has been placed on treating corneal astigmatism at the time of cataract surgery.
For surgeons beginning to add LRIs to their skill set, it may be preferable to start with peribulbar anesthesia and conventional monofocal IOLs, as patients implanted with presbyopia-correcting IOLs are significantly more sensitive to even minor refractive errors. The astigmatic incisions should be performed at the start of the case, while the eye is firm, before any manipulation takes place or dehydration of the cornea occurs due to instrumentation or the operating microscope.
It is a good idea to mark the cornea, especially for large cylindrical errors. To create an incision, the episclera is grasped at the limbus with 0.12-mm forceps approximately 180º away from the intended incision site. Approaching perpendicular to the cornea, a diamond knife with a preset depth guard is advanced into the cornea 0.5 mm central to the limbus, centered on the axis as determined by vector analysis of residual cylinder. Multiple companies manufacture a variety of preset diamond knives. My preference is for a 0.6-mm preset depth.
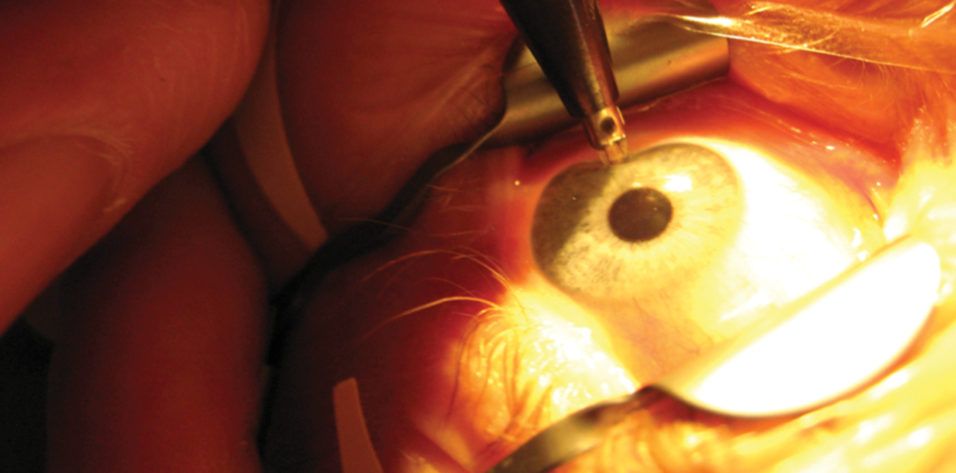
After it is advanced to the desired depth, the knife is held in position for 1 full second to ensure that the full depth of the blade is achieved (Figure 2). Creation of a shallow, ineffective incision is one of the most common mistakes for novice surgeons. The incision is then extended to its desired length. For control purposes, it is always preferable to cut toward oneself.
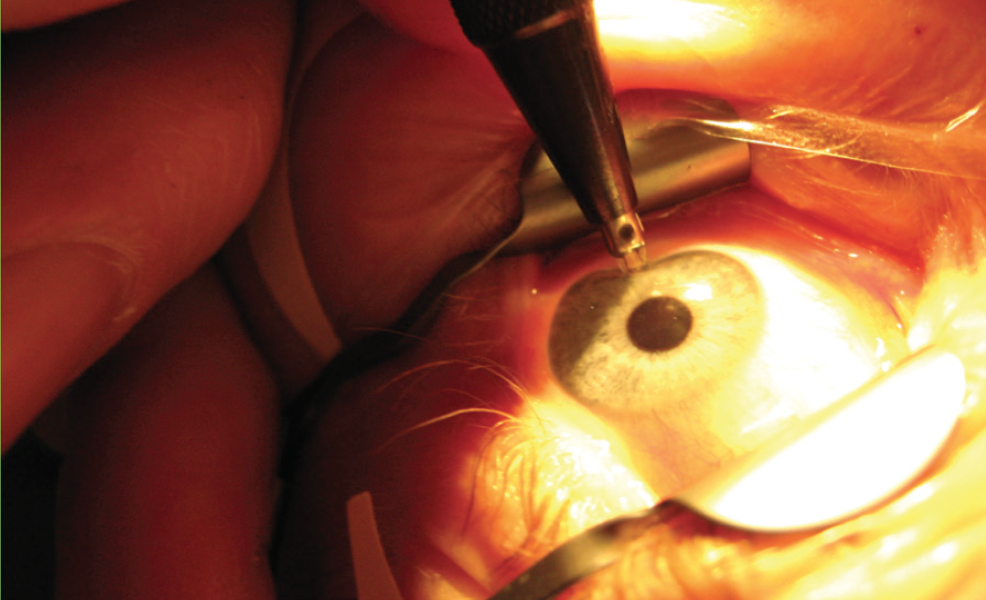
Figure 2. LRI performed at the microscope.
After the surgeon becomes comfortable with the technique, astigmatic incisions can be employed on any patient undergoing cataract surgery, especially those who are likely to end up with 0.50 D or more of residual cylinder.
AT THE SLIT LAMP
Alternatively, experienced surgeons may elect to perform LRIs as an in-office, standalone procedure under the microscope or at the slit lamp. Slit-lamp LRIs are a 30-second procedure, and typically patients walk out of the room seeing better than they did entering.
To perform LRIs at the slit lamp, the phoropter is used to locate the incision axis and then placed adjacent to the patient’s eye with the cylinder stripe aligned on the steep axis of astigmatism. Lidocaine gel is administered into the operative eye, and the patient should be comfortable with his or her head placed forward against that slit lamp’s headband. With an angled preset diamond knife coming from the side, the surgeon performs the procedure as previously described (Figure 3). Postoperatively, a regimen of topical antibiotics and antiinflammatory drops four times daily for 5 days is recommended.
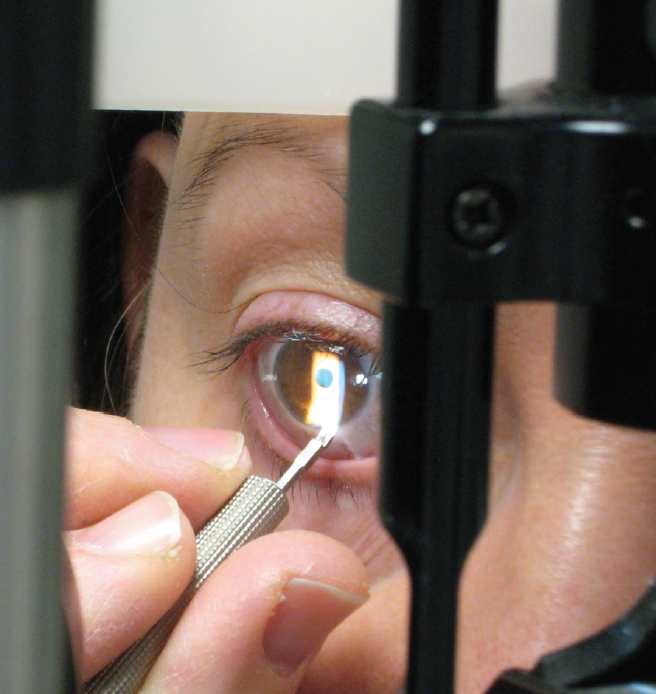
Figure 3. LRI performed at the slit lamp.
COMPLICATIONS
As with any surgical procedure, there are potential complications associated with astigmatic incisions, but most are temporary or correctable. Possible complications include overcorrection, undercorrection, perforation of the cornea, infection, decreased corneal sensation, dry eye, irregular astigmatism, and discomfort. Glare or starbursts are generally not associated with LRIs, but they may be experienced by patients after AKs.
For both under- and overcorrection, I recommend waiting for the refraction to stabilize. A waiting period of 1 to 2 months is typically adequate; however, this is highly surgeon-dependent. In patients with significant remaining astigmatism, it may be necessary to re-treat by deepening or enlarging the original incision. For over-corrected patients, the original incision should be cleaned with the assistance of a Sinskey hook and then partially sutured closed with 10-0 nylon or polypropylene suture.
Placing additional LRIs perpendicular to the original incision for consecutive cylinder without suturing the original incision is not recommended, as this may induce irregular astigmatism. In the event of a corneal perforation, any incision that is not self-sealing may need a 10-0 nylon suture.
CONCLUSION
Astigmatic corneal surgery with a diamond knife can dramatically improve the refractive results of cataract surgery. Astigmatic corneal surgery can be performed intraoperatively or postoperatively in order to titrate residual corneal cylinder.
The most common rate-limiting factor for refractive results after cataract surgery is residual astigmatism, and astigmatic incisional corneal surgery is often the best solution to improve patients’ refractive results and overall satisfaction.