
Cataract and refractive surgeons are aware of the implications of ocular surface disease (OSD) in cataract and refractive surgery. Poor corneal surface health preoperatively can adversely affect the accuracy of biometric measurements on which optimal surgical results depend; postoperatively, it can affect visual quality. Preexisting OSD can lead to poor visual outcomes, symptoms, and overall dissatisfaction.
When members of the ASCRS Cornea Clinical Committee found that many respondents to our annual clinical survey were unfamiliar with current guidelines and modern diagnostic tests and treatments for OSD, we decided to do something. For my colleagues and me on the committee, the goal was to address these educational gaps by developing a new consensus-based practical diagnostic OSD algorithm. We hoped this algorithm would help surgeons to efficiently diagnose and treat visually significant OSD (VS-OSD) before any form of refractive surgery is performed.1
Our algorithm is unique in that it specifically targets the presurgical patient, recognizing that an aggressive treatment approach is required to minimize the delay before surgery. To simplify diagnostic decision-making, we provide a listing of preoperative tests that we consider essential and those we consider optional. To guide surgeons in prioritizing therapy, we categorize OSD as visually significant and non–visually significant (NVS-OSD).
SYNTHESIZED, FOCUSED STRATEGY
Surgeons need a healthy ocular surface in order to deliver accurate outcomes for patients and to ensure their satisfaction with surgery. The strategy we devised is intended specifically for care of the perioperative refractive surgery patient. It is based on ASCRS Cornea Clinical Committee members’ consensus on preferred practices and on an extensive literature review. We do not view our recommendations as competitive to those of other groups; rather, our approach synthesizes and adapts much of the previous excellent work.
Notably, our algorithm is made to be used even if the patient does not complain of OSD symptoms. We know that many older patients with significant cataracts do not have symptoms or do not report them on traditional questionnaires. Additionally, it is known that signs and symptoms of dry eye disease (DED) are poorly correlated and that DED is more pronounced in this population.
NEW HYBRID QUESTIONNAIRE
We created the ASCRS-Modified Preoperative OSD Standardized Patient Evaluation of Eye Dryness (SPEED II) questionnaire (Figure), which to the best of our knowledge, is the first questionnaire designed specifically for preoperative refractive surgery patients. We added extra questions to the original SPEED questionnaire to help screen for other non-DED subtypes of OSD that are relevant in the refractive setting, such as anterior and posterior blepharitis, contact lens intolerance, and atopic and allergic disorders.
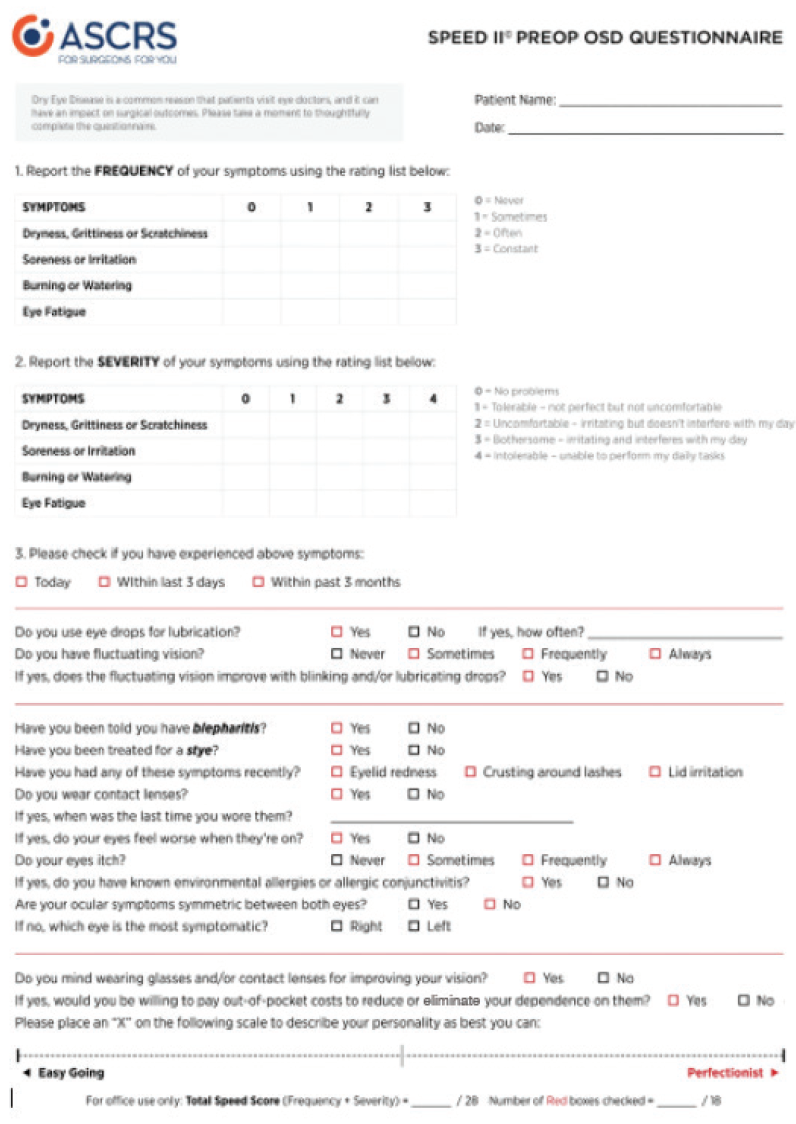
Figure. The modified questionnaire devised by the ASCRS Cornea Clinical Committee.
To address the interplay between patient expectations and the implications of paying out of pocket for premium technology, we adapted items from the Cataract and Refractive Lens Exchange Questionnaire developed by Steven J. Dell, MD.
NONINVASIVE OBJECTIVE TESTING
Independent of the questionnaire’s findings, technicians can proceed with noninvasive objective testing of the patient for refractive and IOL measurements, which also can be used to detect signs of OSD. Our algorithm narrows the initial screening to two essential assessments: tear osmolarity and the inflammatory marker matrix metalloproteinase 9 (MMP-9). These two point-of-care tear tests are relatively inexpensive and can be rapidly performed by trained technicians, and they are sensitive and specific for diagnosing DED.
Osmolarity. Tear hyperosmolarity is central to the modern definition of DED.2 The microchip test card of the TearLab Osmolarity System (TearLab) or other osmometer collects a 50-nL tear sample from the lower lateral tear meniscus, which is used to assess tear osmolarity. The sensitive threshold of 307 mOsm/L differentiates between normal patients and those with mild or moderate DED; an intereye difference greater than 7 mOsm/L is also considered abnormal. In general, mild to moderate DED is typically diagnosed at a mean osmolarity of 315 mOsm/L and severe DED at a mean value of 336 mOsm/L. Intereye variability and day-to-day variability have also been shown to correlate with increasing DED severity.3
MMP-9. The enzyme MMP-9 plays a key role in the breakdown of the ocular surface.4 With a tear sample from the patient, the InflammaDry test (Quidel) takes 10 minutes to determine MMP-9 level. A reading is considered positive if MMP-9 level is 40 ng/mL or greater.5 This metric can be directly related to treatment decisions. Patients with inflammation will likely benefit from preoperative topical antiinflammatory therapy, such as corticosteroids and/or lifitegrast ophthalmic solution 5% (Xiidra, Shire) or cyclosporine ophthalmic emulsion 0.05% (Restasis, Allergan).
Our algorithm, like others, recommends refraining from punctal occlusion for DED until MMP-9 is normalized. This is known as the dirty dishwater concept.
START INFERRING THE DIAGNOSIS
Together, osmolarity and MMP-9 measurements are valuable for identifying OSD in asymptomatic preoperative cataract surgery patients and for inferring potential diagnoses of OSD subtype when considered in the context of symptoms.6
If any one of the three components evaluated up to this point is abnormal, then the presurgical patient is at risk for OSD. Further diagnostic tests can be done to identify OSD subtypes, with both noninvasive (preferred) and invasive options. Although not fundamental to the algorithm, the optional objective tests include measurement of lipid layer thickness, meibography, noninvasive tear breakup time, quantification of tear meniscus height, tear lactoferrin levels, topography or tomography, aberrometry, and objective scatter index (HD Analyzer, Visiometrics).
COMPLETING THE ALGORITHM
Clinical exam. The physical examination rounds out the algorithm, no matter the results of the screening tools. All algorithms are helped by a mnemonic, so we recommend thinking of look, lift, pull, push for the quick focused ocular surface examination to confirm the subtype, severity, and visual significance of OSD (see Look, Lift, Pull, Push Examination below).
Look, Lift, Pull, Push Examination*
- Look. Look at the patient’s blink quality and quantity; examine the eyelids for malposition, lagophthalmos, proptosis and exposure, entropion or ectropion, and trichiasis; then visually assess the tear meniscus height. Look for signs of anterior and posterior blepharitis. Look at the interpalpebral ocular surface and at the interpalpebral cornea. In some cases, punctate epithelial erosions and superficial punctate keratitis can be seen under direct illumination without dyes or stains.
- Lift and pull. Lifting up and then pulling out the upper eyelid is an often overlooked portion of the ocular surface examination. This maneuver can detect superior limbal keratitis and superior corneal scars, but the main reasons for lifting and then pulling the upper lid are to rule out superior epithelial basement membrane dystrophy and to identify eyelid laxity and floppy eyelid syndrome.
- Push. Pushing on the lower lid margin expresses the meibomian glands, allowing the quality, quantity, and flow of the meibum to be assessed. Gland expression can be particularly helpful in identifying patients with nonobvious meibomian gland dysfunction, a form of obstructive dysfunction in which classic inflammatory signs are absent.
* Seventy percent of ASCRS Cornea Clinical Committee members stated that they were comfortable allowing a trained physician extender (eg, technician or physician assistant) to perform this step.
Final phase. At this stage in the algorithm, symptoms have been assessed, baseline refractive measurements and noninvasive OSD tests have been completed, and the ocular surface has been examined and stained for visual evidence of disease. With this basket of information, the clinician can assess whether or not the patient’s OSD is visually significant with a potential for adverse effect on surgical outcomes.
TREATMENT
For any patient with VS-OSD, preoperative refractive measurements and the surgery itself should be postponed until the OSD is sufficiently treated and converted to NVS-OSD. For patients with NVS-OSD, surgery can proceed as planned; however, patients should receive education and have their expectations managed.
The ASCRS Cornea Clinical Committee members agreed that treatment of VS-OSD in preoperative patients requires an aggressive and multifaceted approach to speed the process and minimize surgical delays. To that end, we advocate beginning at step 2 or later of the Tear Film and Ocular Surface Society’s Dry Eye Workshop II (TFOS DEWS II) treatment guidelines.7 A combination of medical and procedural interventions based on disease subtype and severity will dictate the best approach for the preoperative patient.
As DED is widely recognized as a multifactorial disease involving tear composition, ocular surface inflammation, and lid margin disease, there is an ever-growing array of therapies available. Some of the options are outlined here.
Inflammation. In both aqueous deficient and evaporative DED, antiinflammatory treatment can be beneficial. Pulsed topical steroids may be considered in the short term. Prescription topical antiinflammatory drugs, such as cyclosporine and lifitegrast, have been shown to be effective in long-term management of DED. If ocular rosacea and lid margin inflammation are present, oral tetracyclines can be considered.
Lid margin disease. Meibomian gland dysfunction (MGD) and anterior blepharitis must be treated before surgery. Relieving obstruction in the meibomian glands must be part of therapy to improve DED symptoms. Blepharitis is a common cause of cataract surgery cancellation and a major risk factor for postoperative endophthalmitis.
Home-care compliance is notoriously low, and therefore antiinfective therapies should be initiated aggressively before surgery. Hypochlorous acid solutions can be of benefit. For Demodex infestation, lid scrubs that include the ingredient tea tree oil should be applied. In-office treatments such as mechanical blepharoexfoliation of the lid margin (BlephEx, Scope Ophthalmics) or thermal pulsation with devices including the LipiFlow (Johnson & Johnson Vision), iLux (Alcon), MiBo ThermoFlo (Mibo Medical Group) or TearCare (Sight Sciences) can be offered. Intense pulsed light therapy, originally developed for patients with acne or rosacea, is being used off-label for chronic MGD with some success.
Increasing dietary intake of omega-3 fatty acids may also help improve lid health and the quality of oil secretions.
Abnormal corneal staining. Aggressive lubrication with preservative-free artificial tears should be initiated when the patient exhibits significant punctate staining. Neurostimulation (TrueTear, Allergan) has been shown to promote aqueous, mucin, and meibum secretion; to improve punctate staining; and to positively affect DED symptoms. The use of autologous serum drops may also be considered.
A self-retaining amniotic membrane or therapeutic bandage contact lens can be used preoperatively to address severe punctate keratitis and to restore a smooth ocular surface. Human amniotic membrane transplantation has become another alternative technique for some types of OSD. The ability to place a self-retaining cryopreserved amniotic membrane has expanded the use of this option in the clinic. Bandage contact lenses and punctal occlusion are useful in patients with low tear volume and corneal staining.
Eyelid abnormalities that lead to corneal exposure should also be treated preoperatively. Environmental modifications can go a long way, as can preoperative patient education. Patients should be made aware that any form of OSD can worsen and become visually significant after surgery.
AVOID CERTAIN MEDICATIONS
In our report, we also remind surgeons that many systemic medications can contribute to worsening DED, so it is important to review medications and discontinue offending agents when possible. Declining hormone levels, both estrogen and androgen, in the elderly can trigger significant DED symptoms. Limited evidence indicates that topical hormone treatment can improve DED symptoms.8
In patients with superficial abnormalities of the corneal surface leading to topographic irregular astigmatism (ie, lumps and bumps), a procedural intervention may be indicated.
CONCLUSION
This project was initiated in response to significant educational gaps identified in recent ASCRS clinical surveys. Although more than 90% of respondents to these surveys recognized that even mild to moderate DED can affect patient satisfaction after cataract and refractive surgery, less than 10% reported using modern techniques for identifying and treating OSD in their routine preoperative assessments.
In light of these survey findings, we tailored our approach to target the preoperative refractive surgery patient, who depends on accurate and efficient OSD diagnosis and treatment for rapid reversal. No one wants to delay surgery, but everyone wants excellent outcomes.
1. Starr CE, Gupta PK, Farid M, et al; ASCRS Cornea Clinical Committee. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg. 2019;45(5):669-684.
2. [no authors listed]. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5(2):75-92.
3. Lemp MA, Bron AJ, Baudouin C, et al. Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol. 2011;151(5):792-798.e1.
4. Sambursky R, Davitt WF III, Friedberg M, Tauber S. Prospective, multicenter, clinical evaluation of point-of-care matrix metalloproteinase-9 test for confirming dry eye disease. Cornea. 2014;33(8):812-818.
5. Sambursky R, Davitt WF III, Latkany R, et al. Sensitivity and specificity of a point-of-care matrix metalloproteinase 9 immunoassay for diagnosing inflammation related to dry eye. JAMA Ophthalmol. 2013;131(1):24-28.
6. Sullivan BD, Whitmer D, Nichols KK, et al. An objective approach to dry eye disease severity. Invest Ophthalmol Vis Sci. 2010;51(12):6125-6130.
7. Craig JP, Nelson JD, Azar DT, et al. TFOS DEWS II report executive summary. Ocul Surf. 2017;15(4):802-812.
8. Worda C, Nepp J, Huber JC, Sator MO. Treatment of keratoconjunctivitis sicca with topical androgen. Maturitas. 2001;37(3):209-212.




