Posterior capsular opacification (PCO) is the most common postoperative complication of cataract surgery. Long-term studies have shown that 4% of patients will have this indication at 3 years postoperative, increasing to 12% at 5 years and 42% at 10 years.1 It is more common in patients younger than 65 years, which is an important consideration for patients undergoing refractive lens exchange, as they are generally of this age group.
The development of PCO is a concern for several reasons. Even a small amount of PCO can cause a loss of quality of vision,2 and this is particularly true for patients with multifocal IOLs. Occurrence of PCO necessitates extra visits for assessment, Nd:YAG laser capsulotomy, and follow-up, and there can be adverse events for the eye after laser capsulotomy.3 Furthermore, laser capsulotomy adds costs to the health care system, and it is unavailable in many parts of the developing world where Nd:YAG lasers are scarce.
VALUE OF PPC
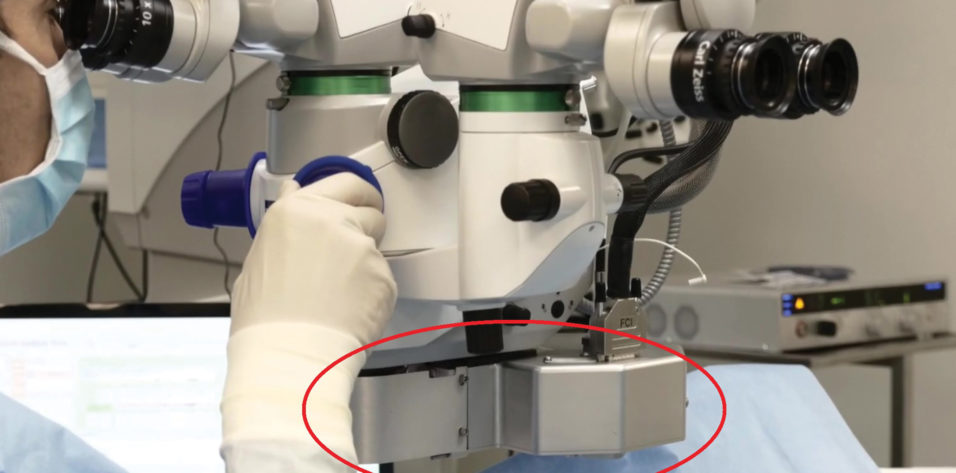
As other articles in this issue of CRST make clear, creating a primary posterior capsulotomy (PPC) has a number of potential advantages if the aforementioned issues are to be avoided. Marie-José Tassignon, MD, PhD, has, for a number of years, demonstrated the advantages of a PPC performed in conjunction with her bag-in-the-lens approach (Figure 1).4
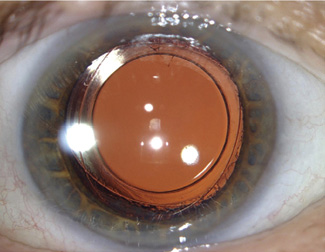
Figure 1. Bag-in-the-Lens IOL with PPC at 4.5 years postoperative.
Still, there is a reluctance among most cataract surgeons to consider routine PPC. This is usually because of two reasons: (1) There is a perceived risk for vitreous loss; and (2) creation of the PPC is more difficult than creation of the anterior capsulotomy.
It is possible that, if PPCs could be easily and consistently created, this attitude would change.
Schojai et al have described the use of a femtosecond laser to create PPCs at the end of cataract surgery.5 To do this, they take the patient back to the femtosecond laser, reapply the patient interface, and trick the laser into thinking it is firing at the anterior capsule because the laser software does not yet support performing PPC.
ANOTHER APPROACH
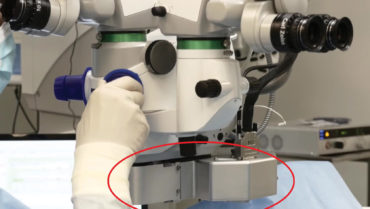
There is another laser approach on the horizon. The CapsuLaser (Excel-Lens) is a laser that can be affixed to the binocular indirect connection points of any operating microscope (Figure 2). The laser wavelength requires a target, which is created by staining the anterior capsule with an enhanced solution of trypan blue dye (CapsulBlue, Excel-Lens).
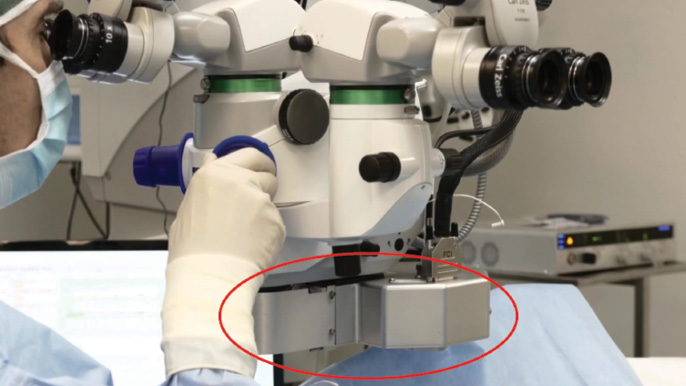
Figure 2. CapsuLaser attached under the operating microscope.
After the capsule is stained, the eye is filled with an optically clear OVD, a specially manufactured sodium hyaluronate 2% solution (CapsulVisc, Excel-Lens). A patient interface is then placed, and the laser is focused by the surgeon. The patient assists with centration by looking at a fixation light.
When the laser is activated, it takes 1 second to create the capsulotomy (Figure 3), which can be sized from 4.5 to 6.0 mm in 0.1-mm increments. The type IV collagen of the capsule absorbs the laser energy and is converted into amorphous collagen. The edge of the capsular opening is then rolled over (Figure 4), and it is much more elastic than a normal capsulotomy edge because of the amorphous collagen. This was shown in a study using paired cadaver eyes in a laboratory experiment. (unpublished data)

Figure 3. CapsuLaser creates an anterior capsulotomy in 1 second.
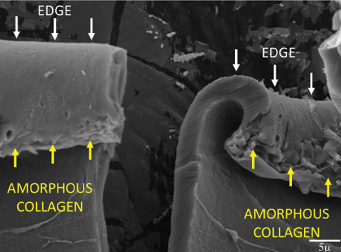
Figure 4. A cut capsulotomy edge shows the change in collagen caused by the laser energy.
The laser has been used successfully for anterior capsulotomy in more than 500 patients, and the device received the CE Mark in 2018.
Anterior capsulotomy with CapsuLaser was compared against manual curvilinear continuous capsulorhexis in a prospective study and was shown to be superior for sizing, circularity, and centration.6 Also, there were 100% free capsulotomy caps, and there was 100% 360º capsulotomy coverage of the IOL, which is important for PCO prevention.
ASSESSING CAPSULASER FOR PPC
The idea of using CapsuLaser for PPC is attractive because it can be performed during the course of a routine cataract procedure with minimal change in the flow of the operation. The feasibility of using this laser for PPC has been assessed in several ways in the laboratory setting.
First, in a porcine eye, the posterior capsule was exposed to trypan blue, the dye was washed out, and the capsular bag was filled with the same OVD used for anterior capsulotomy with CapsuLaser. The laser was then fired to create a 4-mm opening (Figure 5), and the capsulotomy disc was removed. (The opening could be made any size from 4.5 to 5.5 mm.)
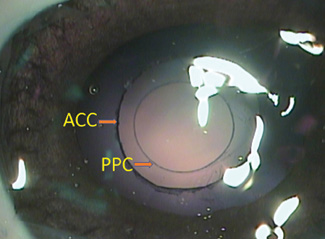
Figure 5. Anterior and posterior capsulotomies made with CapsuLaser in a porcine eye.
In order to assess whether a PPC could be created through an IOL, the laser was used to make an anterior capsulotomy through a phakic IOL in a patient who was about to undergo cataract surgery. The dye was injected under the phakic IOL, it was washed out, and the anterior chamber was filled with OVD as usual. The laser was activated as described earlier, and the anterior capsulotomy formed as usual, but behind the phakic IOL (Figure 6).

Figure 6. CapsuLaser anterior capsulotomy created through a phakic IOL in a patient scheduled for cataract surgery.
The next approach, given the possible use of the Bag-in-the-Lens (BIL, Morcher; not FDA approved) IOL, was to remove the natural lens, stain the posterior capsule, and implant the BIL in a porcine eye. Once this was done, the posterior capsule was lasered (Figure 7), and the BIL was maneuvered into position.

Figure 7. PPC created behind a BIL in a porcine eye.
Even if a BIL is not used and posterior optic capture of a standard IOL is desired, CapsuLaser could be useful. The posterior capsule, although thinner than the anterior capsule, is more elastic. The edge of a PPC created with CapsuLaser is similar in appearance to that of the anterior capsule (Figure 8).
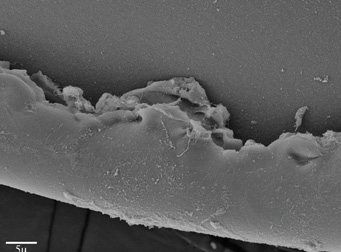
Figure 8. Scanning electron microscope photograph of a PPC disc edge.
Certain issues remain to be resolved in relation to using this laser for PPC:
First, when should staining of the posterior capsule be done: directly after irrigation and aspiration or under OVD? Once the dye has been washed out, the bag could be filled with OVD to allow IOL implantation. The OVD would then have to be removed from behind the IOL, as it is important that the posterior capsule not be concave but also not be pushed too far superiorly.
Second, is the retina safe if the laser energy is directed farther posteriorly? The safety profile of the laser ensures that its beam has diverged widely by the time it reaches the retina. Although the posterior capsule is a little farther posterior than the anterior capsule of an intact lens, the beam still diverges safely by the time it reaches the retina (Figure 9).
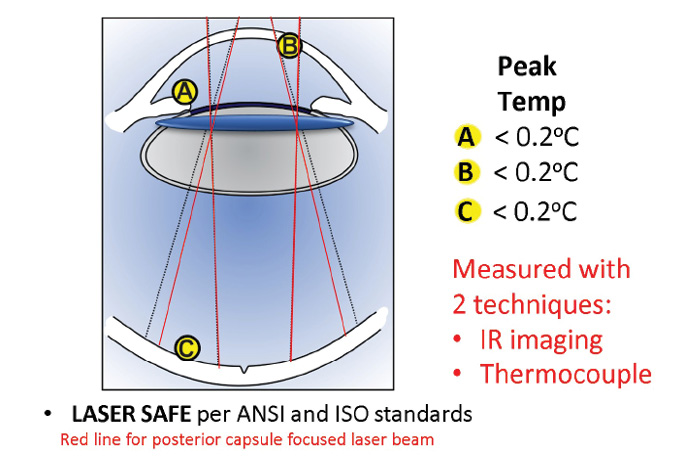
Figure 9. Safety profile for CapsuLaser. The beam diverges widely by the time it reaches the retina.
Third, what happens to the posterior capsular disc? Schojai et al reported that they did not need to remove the PPC disc created with a femtosecond laser,5 but we do not know if the same will apply with the disc created with CapsuLaser. Of course, with this laser, the scenario would be easier to deal with, as the eye is still open and the IOL has yet to be finally positioned.
Fourth, in order to place the IOL behind the posterior capsule in Berger space, will OVD be required? Drs. Marie-José Tassignon and Rupert Menapace do not currently use any OVD to do this with their respective techniques.7
CONCLUSION
Although no human use of CapsuLaser for PPC has yet occurred, the basics of the likely technique have been developed in the laboratory, as described in this article. It is expected that this technique will be put into practice in the near future.
1. Vock L, Menapace R, Stifter E, et al. Posterior capsule opacification and neodymium:YAG laser capsulotomy rates with a round-edged silicone and a sharp-edged hydrophobic acrylic intraocular lens 10 years after surgery. J Cataract Refract Surg. 2009;35(3):459-465.
2. Yotsukura E, Torii H, Saiki M, et al. Effect of neodymium:YAG laser capsulotomy on visual function in patients with posterior capsule opacification and good visual acuity. J Cataract Refract Surg. 2016;42(3):399-404.
3. Billotte C, Berdeaux G. Adverse clinical consequences of neodymium:YAG laser treatment of posterior capsule opacification. J Cataract Refract Surg. 2004;30(10):2064-2071.
4. Tassignon MJ, De Groot V, Vrensen GF. Bag-in-the-lens implantation of intraocular lenses. J Cataract Refract Surg. 2002;28(7):1182-1188.
5. Schojai M, Schultz T, Haeussler-Sinangin Y, et al. Safety of femtosecond laser-assisted primary posterior capsulotomy immediately after cataract surgery. J Cataract Refract Surg. 2017;43(9):1171-1176.
6. Stodulka P, Packard R, Mordaunt D. Clinical investigation of an innovative selective laser device to assess its efficacy and safety for the creation of anterior capsulotomies in cataract patients. Paper presented at: ESCRS Annual Meeting; September 22-26, 2018; Vienna, Austria.
7. Tassignon MJ, Jones J, Oetting T, et al. Mastering the posterior capsule: thinking out of the bag paradigm shift. Course presented at: AAO Annual Meeting; October 26-30, 2018; Chicago, IL.