Many Factors Involved in Toric IOL Selection
by Balamurali K. Ambati, MD, PhD, MBA

Ophthalmologists now enjoy a variety of toric IOL options. Among the available models, the types I use include the Tecnis Toric 1-Piece (ZCT series, Johnson & Johnson Vision), the Acrysof IQ Toric (SN and SA series, Alcon), and the enVista toric (MX60T series, Bausch + Lomb) IOLs. Each of these companies also offers presbyopia-correcting toric IOLs. I will not discuss the presbyopia-correcting toric lenses here; that is a much longer and deeper conversation with patients.
I try to choose the IOL that I feel will be the best for each patient based on lifestyle desires, visual needs, and the circumstances of their eyes. For example, if a patient has had myopic LASIK, I prefer the Tecnis Toric lenses, which have the greatest negative spherical aberration. For a patient who has had hyperopic LASIK, the SA series from Alcon has the most positive spherical aberration to counteract the hyperopic LASIK aberrations. A postradial keratotomy patient, or a patient with mild Fuchs dystrophy or mild corneal scarring, may be best off with the Bausch + Lomb lenses, which have no spherical aberrations and have a bit longer defocus range and therefore a broader landing zone on the spherical equivalent target. A patient with mild drusen may be best served with blue-light–blocking SN lenses from Alcon.
For patients with axial lengths greater than 24.5 mm, I generally insert a capsular tension ring to minimize rotation of the toric IOL, to which unfortunately the Tecnis lenses in particular are prone. Patients with low amounts of cylinder can be treated with an enVista toric with +1.25 D of cylinder, which treats as little as 0.83 D of corneal cylinder, whereas patients with high cylinder are better off with the high-diopter Tecnis Toric models.
Placement and width of the corneal incision are also important considerations in surgical planning. The length of the eye can affect the toric performance of an IOL. If the IOLMaster (Carl Zeiss Meditec) or Lenstar (Haag-Streit) printout shows that each 0.50-D step changes the refractive outcome by 0.40 D or 0.25 D, rather than the typical shift of 0.33 to 0.35 D, this indicates that the toric effectivity ratio of 0.68 is shifted up or down accordingly.
I generally like to compare three sets of keratometric readings (Lenstar, Scheimpflug photography, and autokeratometry readings). I have my technicians repeat scans if necessary to try to achieve concordance. If a patient’s ocular surface is not optimized, we treat the patient’s dry eye and blepharitis prior to obtaining repeat scans.
Seeking the Best Quality of Vision
by Daniel H. Chang, MD

When selecting a toric IOL for a patient who desires good uncorrected distance visual acuity after surgery, my primary goal is to provide the patient with the best possible quality of vision. The quality or sharpness of vision is largely determined by the presence or absence of optical aberrations, which can be influenced by IOL material and design. Even among monofocal toric IOLs, there is a range of optical quality, and a presbyopia-correcting toric lens introduces further potential for optical compromises.
My go-to toric IOLs are the Tecnis Toric IOLs—both the Tecnis Toric monofocal IOL for correction of astigmatism and the Tecnis Symfony Toric (Johnson & Johnson Vision) extended depth of focus (EDOF) IOL for correction of astigmatism and presbyopia.
CORRECTION OF OPTICAL ABERRATIONS
All Tecnis IOLs have aspheric optics to correct the +0.27 µm of spherical aberration (SA) of the average cornea. The Tecnic Toric models are the only toric IOLs to provide a full -0.27 µm of negative SA to reduce net SA to essentially zero in the pseudophakic eye. Therefore, these IOLs provide sharp vision as well as enhanced functional vision and safety.
Tecnis Toric IOLs are also made from the lowest dispersion hydrophobic acrylic material on the market, with an Abbe number of 55, to minimize the amount of longitudinal chromatic aberration (CA) in the pseudophakic eye. CA can be measured by the difference in refraction between red (700 nm) and violet (400 nm) wavelengths at either end of the spectrum of visible white light. The cornea has a baseline aphakic CA of 1.69 D.1 All refractive lenses add CA to an optical system, so it is important for an IOL to add as little CA as possible. Depending on the dispersion of the IOL material, it can potentially increase or decrease the eye’s CA relative to the natural lens.
Colleagues and I performed optical bench testing of the various materials used in toric IOLs available in the United States.2 We found that there is a nearly threefold difference in the amount of CA introduced by these toric IOLs (Figure 1) and that the Tecnis Toric IOL adds the least (0.47 D), at a level comparable to that of the natural human lens.
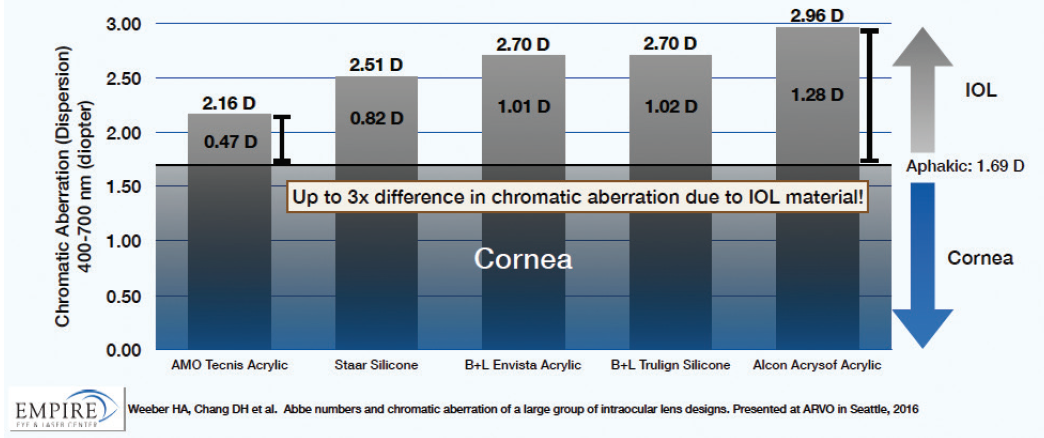
Figure 1. CA of toric IOLs. There is a nearly threefold difference in the amount of CA introduced into the eye by the optic materials of different toric IOLs.
Design features of the Tecnis Symfony Toric IOL further reduce CA. In this lens, diffractive achromatic technology similar to that used in high-end diffractive-optics camera lenses corrects the overall CA of the eye’s optical system. This helps to enhance contrast sensitivity and improve retinal image quality.
Simultaneously correcting both SA and CA has been shown to provide better quality of vision than reducing only one or the other. We see this in the excellent visual quality, particularly at night, with the monofocal Tecnis IOL, as represented by modulation transfer function (MTF). MTF is a measure of the amount of contrast transferred by the optics in a visual system. The higher the MTF value, the higher the image contrast. In laboratory bench studies, the Tecnis monofocal platform had a 16% higher MTF value under photopic conditions and a 38% higher MTF value under mesopic conditions than a leading monofocal toric platform. The MTF of the Tecnis Symfony presbyopia-correcting IOL, an EDOF design, was 35% higher in photopic conditions and 74% higher in mesopic conditions than the only available multifocal toric IOL platform (Figure 2).3
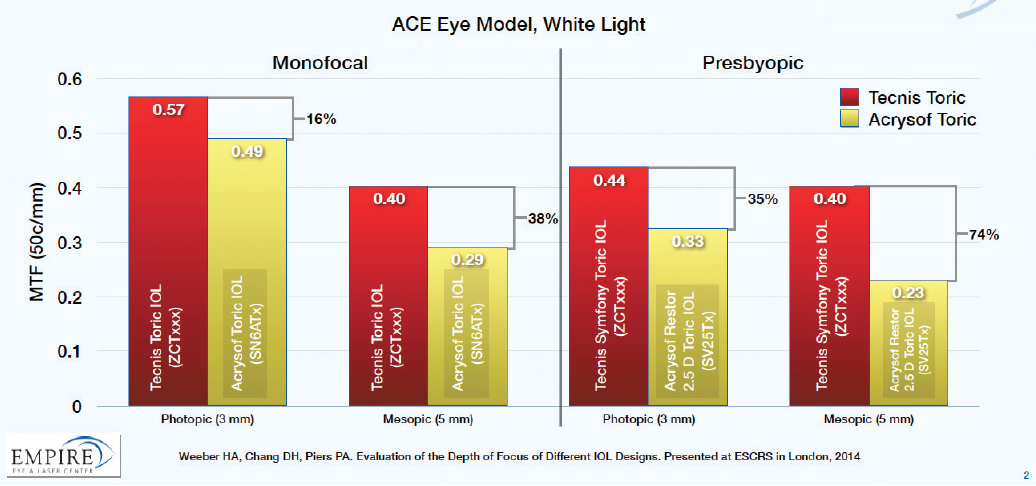
Figure 2. Image quality of toric IOLs. Image contrast, as measured by MTF, can vary by up to 38% in monofocal and 74% in presbyopia-correcting designs.
Quality of vision can also be affected by postoperative changes in the IOL and the ocular environment. I prefer the Tecnis toric IOLs because their lens material has not been associated with significant glistenings, which can cause light scatter and reductions in image contrast.4,5 It also has a lower rate of severe capsular phimosis compared with other toric IOL platforms.6
Choosing an IOL that provides the highest possible image quality for the patient increases the chance that the patient will be able to tolerate other factors that affect vision or visual quality, including residual refractive error, ocular surface problems, posterior capsular opacification, and minor retinal pathology.
ROTATIONAL STABILITY
I have found that Tecnis toric IOLs offer a balance of ease of handling and stability. The lenses are easy to position within the capsular bag, and, with careful surgical technique, positional and rotational stability are excellent. I return to the OR to reposition only about one in 100 toric IOLs.
Technique factors related to good positioning and stability include meticulous wound construction; a well-sized and centered capsulorhexis; complete unfolding of the lens with proper alignment of the axis; removal of OVD at the end of surgery, including from behind the lens; and a well-sealed wound. Postoperative wound leakage may result in hypotony, and a soft eye can allow external factors (eg, eye rubbing) to exert rotational force on the IOL. I believe that most surgeons will realize greater gains in rotational stability by improving surgical technique than by selecting another type of toric IOL that may have inferior optical characteristics.
CORRECTION OF PRESBYOPIA
I encourage all my astigmatic patients to opt for a toric IOL so that they can maximize their uncorrected distance visual acuity. Another major goal of mine is to reduce patients’ needs for bifocal spectacles after surgery, as these have been shown to more than double the risk of falls in the elderly.7 For patients who choose to pay out of pocket for better visual outcomes, many would like greater spectacle independence at all distances, which is possible with a toric presbyopia-correcting lens. For these patients, I prefer the Tecnis Symfony Toric IOL because it provides all the optical quality benefits I outlined earlier, plus a functional range of near and intermediate vision without glasses.
With the Tecnis Toric and Tecnis Symfony Toric IOLs, patients with astigmatism can enjoy greater spectacle independence after surgery. For the occasional patient who has residual refractive error after surgery, whatever the reason, many modalities are available to improve their UCVA. Because there is no easy fix for poor visual quality stemming from poor IOL optical quality, I prefer to use the Tecnis toric platform, which I believe provides the highest possible optical quality for my patients.
1. Zhao H, Mainster MA. The effect of chromatic dispersion on pseudophakic optical performance. Br J Ophthalmol. 2007;91:1225-1229.
2. Chang DH, Weeber HA, Lowery MD, Piers PA. Chromatic aberration of intraocular lenses measured in vitro and in vivo. Paper presented at: Association for Research in Vision and Ophthalmology Annual Meeting; May 1-5, 2016; Seattle, WA.
3. Weeber HA, Chang DH, Piers PA. Evaluation of the depth of focus of different IOL designs. Paper presented at: European Society of Cataract and Refractive Surgeons Annual Meeting; September 13-17, 2014; London, United Kingdom.
4. Nagata M, Matsushima H, Mukai K, et al. Clinical evaluation of the transparency of hydrophobic acrylic intraocular lens optics. J Cataract Refract Surg. 2010;36(12):2056-2060.
5. Van der Mooren M, Franssen L, Piers P. Effects of glistenings in intraocular lenses. Biomed Opt Express. 2013;4(8):1294-1304.
6. Kahraman G, Ferdinaro C, Wetzel B, et al. Intraindividual comparison of capsule behavior of 2 hydrophobic acrylic intraocular lenses during a 5-year follow-up. J Cataract Refract Surg. 2017;43(2):228-233.
7. Lord SR, Dayhew J, Howland A. Multifocal glasses impair edge-contrast sensitivity and depth perception and increase the risk of falls in older people. J Am Geriatr Soc. 2002;50:1760-1766.
Different Patients Require Different IOL Solutions
by Jay S. Pepose, MD, PhD

More than half of cataract patients have clinically significant corneal astigmatism amenable to toric IOL correction, and about two-thirds of these patients have low corneal astigmatism that should not be overlooked. Choosing the best IOL is vital to providing a satisfactory outcome for these patients. I currently have different go-to toric IOLs depending on the characteristics of patients and the optical goals they wish to achieve.
In general, when I choose a toric IOL, I first consider rotational stability because every degree of misalignment results in reduction of the correction of astigmatism by 3.3%. This means that a 10º misalignment reduces the cylinder offset by 33%.
FACTORS AFFECTING ROTATION
IOL rotation can be affected by problems with surgical technique, such as OVD left behind the IOL, wounds that are not watertight, or chambers that are left overhydrated, which can allow the IOL to rotate. I try not to create an overlarge anterior capsulorhexis to ensure that there is adequate coverage of the toric IOL, and I generally do not polish the underside of the anterior capsule, except when implanting a hinged plate-haptic toric IOL. In eyes with long axial lengths (which tend to have larger capsular bags that can allow rotation), I consider the use of a capsular tension ring. Because recent studies suggest that most instances of IOL rotation may occur during the first hour postoperatively,1 having the patient rest during the early postoperative period may also be prudent.
Toric IOL rotation is also affected by IOL design and material. The material may contribute to stability by absorbing fibronectin. This quality is particularly high with the AcrySof IQ Toric IOL, which may allow better adhesion of this IOL to the capsular bag and therefore lower rates of posterior capsular fibrosis.
Haptic design also plays a role in stability, and this may be reflected in my experience with the Tecnis family of toric IOLs, which, in my hands and others’,2 has a tendency toward counterclockwise rotation. The need for repositioning is an additional imposition on patients who have paid out of pocket for a toric IOL, and it should be delayed at least 1 week to allow some contraction of the capsular bag.3
The choice of a specific toric IOL is also dependent on biometry (ie, anterior and posterior corneal cylinder, corneal spherical aberration, and other higher-order aberrations), the patient’s visual needs, and whether the patient has had previous keratorefractive surgery.
EXCELLENT STABILITY
My current go-to monofocal toric IOL is the AcrySof IQ Toric. I find that it has excellent rotational stability and seldom needs repositioning. It is available in a broad range of toric powers. I use the Barrett formula to calculate the toric power and position, while taking into account posterior corneal astigmatism.
This aspheric IOL has a negative SA value that offsets most of the positive SA in the average human cornea. This enhances image quality while still allowing some contribution to depth of field and tolerance of small amounts of defocus.
In the United States, we have recently seen the release of the enVista MX60T Toric IOL, which is available with the lowest astigmatic offset, around 0.90 D at the corneal plane. This lens is on a zero-aberration platform, with reports of excellent rotational stability and absence of glistenings.4
There are also patients who seek EDOF correction, and for these patients, my go-to IOL is the Tecnis Symfony Toric. This IOL has a posterior achromatic diffractive surface to enhance image contrast by reducing CA, an echellete design to achieve EDOF, and an anterior toric aspheric surface to offset corneal astigmatism and corneal spherical aberration. The Symfony Toric IOL provides excellent distance and intermediate vision and functional near vision, but I often mix and match this with a multifocal IOL in the nondominant eye to provide more spectacle independence.
I have also had good experience using the AcrySof IQ Restor +2.5 D IOL with Activefocus optical design (Alcon) for patients who desire good distance and intermediate vision while minimizing photic phenomena. This lens has the same rotational stability as the AcrySof IQ monofocal toric.
For patients who have had previous keratofractive surgery, particularly hyperopic LASIK, I generally use the Trulign toric IOL (Bausch + Lomb). This lens provides excellent contrast sensitivity, as it does not split light energy to multiple foci. It is also aberration-free, so it does not add to the negative corneal spherical aberration of patients who have had hyperopic LASIK. The polyimide haptics of the lens provide rotational stability. I use the Barrett toric calculator to determine the correct toric power.
1. Inoue Y, Takehara H, Oshika T. Axis misalignment of toric intraocular lens: placement error and postoperative rotation. Ophthalmology. 2017;124(9):1424-1425.
2. Lee BS, Chang DF. Comparison of the rotational stability of two toric intraocular lenses in 1273 consecutive eyes. Ophthalmology. 2018;125(9):1325-1331.
3. Oshika T, Inamura M, Inoue Y, et al. Incidence and outcomes of repositioning surgery to correct misalignment of toric intraocular lenses. Ophthalmology. 2018;125(1):31-35.
4. Packer M, Williams JI, Feinerman G, Hope RS. Prospective multicenter clinical trial to evaluate the safety and effectiveness of a new glistening-free one-piece acrylic toric intraocular lens. Clin Ophthalmol. 2018;12:1031-1039.
Choice Depends on Patients’ Needs
by Richard S. Davidson, MD

I use two toric IOL models primarily, and my choice depends on the visual needs and desires of the patient. I use the AcrySof IQ Toric as my go-to choice for a monofocal toric IOL, and I use the Tecnis Symfony Toric EDOF IOL as my go-to for a presbyopia-correcting toric IOL.
There are other toric lenses available in the United States, and even more in Europe that US surgeons do not have access to, but these are the two that I use and have the most experience with. Both models are highly reliable, and my choice really depends on the patient’s preferences.
The main characteristics that surgeons look for with toric IOLs are predictability of visual outcome and rotational stability, and both of these lens platforms fit those requirements. Obviously there are other factors to consider, such as ease of implantation and whether the lens can go through a small enough incision, but both of these toric lens platforms are very predictable, with excellent outcomes for our patients. Those are the most important characteristics for me.
I use the Acrysof Toric lens to correct for either distance or near, often with a monovision strategy. If patients want a range of vision correction in both eyes, I use the Symfony toric lens. Out of my total cataract population, I use AcrySof Torics in about 18% of patients and presbyopic correction with the Tecnis Symfony in about 5%.
In making the decision about lens choices, we talk to patients about what type of correction they are looking for. If they are comfortable with monovision—for example, if they have been wearing contact lenses with a monovision prescription—then I use the monofocal AcrySof Toric. If they want that presbyopic correction in both eyes, then I use the Symfony Toric. Both lenses work great, so it really just comes down to the visual needs of the patient.
We make sure in our preoperative discussions that patients understand the differences between the lenses, the potential pluses and minuses, and so forth. This patient education is key because we have many good options and we want patients to make whatever decision is best for them.
Both of these toric platforms are available in a wide range of powers, and they can cover the majority of patients for cylindrical and spherical correction. It is rare to encounter patients who fall beyond the available ranges of cylindrical correction, but it does happen. In those situations, I combine one of the lenses with PRK or laser arcuate incisions to try to reduce the astigmatism as much as possible. I know that, in Europe, there are some toric lenses with custom-ordered expanded ranges that go beyond what we have in the United States, so that is an option for patients with very high degrees of astigmatism. I have not used any of those lenses, but some of our European colleagues have.