Unhappy RK patients present to ophthalmology practices periodically; know how to improve their quality of life.
Late complications of radial keratotomy (RK) can occur, and, for the newest generation of refractive surgeons unfamiliar with this type of incisional surgery, management can be challenging. The goal of this pictorial review is to enhance understanding of the common complications of RK and the rationales for several management approaches.
BACKGROUND
RK, pioneered by Professor Svyatoslav Nikolayevich Fyodorov in 1974, first performed in Russia, and adopted by US surgeons in particular and ophthalmologists in the rest of the world in the mid to late 1980s, was a promising technique for the correction of low myopia. RK relied on the effect of a series of deep radial incisions to relax the peripheral and flatten the central cornea in patients with myopia. The number of incisions varied from four to 16 and sometimes ambitiously 32, depending on the level of correction required, but all incisions extended from the pupil to the corneal periphery in a radial pattern, like the spokes of a wheel.
The RK technique quickly became more sophisticated and relatively more reproducible through the introduction of diamond knives, pachymetry, and nomograms that were based on the patient’s age and level of correction. The Russian technique was felt to be more effective with deeper incisions centrally, however, there was considerable risk of entering the visual axis.
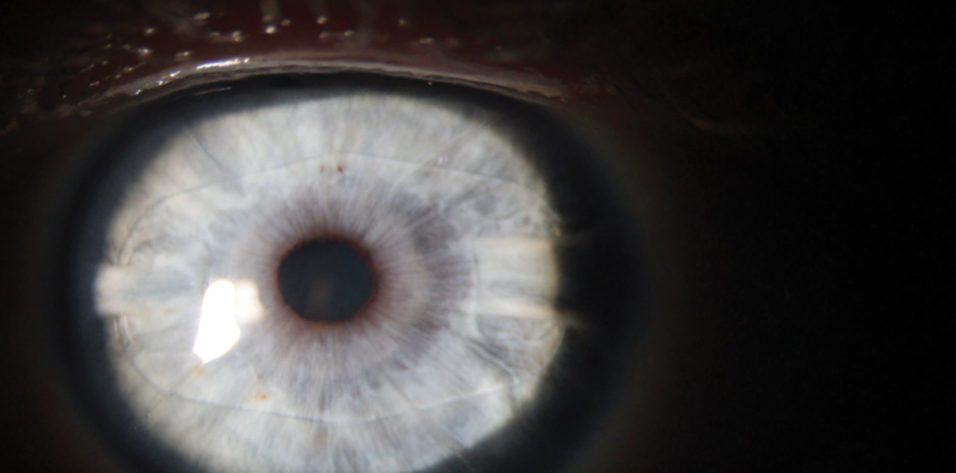
The main determinants of effect of RK were the size of the optical zone, the number of incisions, and the patient’s age. The realization that there was no need to cut to the limbus gave rise to the concept of minimally invasive RK (mini-RK). Introduced by Richard L. Lindstrom, MD, in 1991, mini-RK (Figure 1) minimized the invasiveness of RK by reducing the number, depth, and area of incisions. In mini-RK, incisions extending from the 3- to the 8-mm optical zone were created, rather than the variable number of 11-mm full-length incisions used in the standard RK technique.
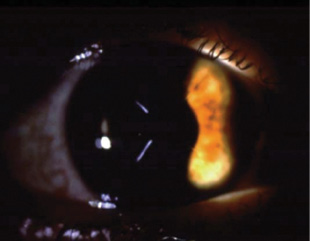
Figure 1. This eye underwent mini-RK.
I was Dr. Lindstrom’s fellow in Minneapolis at that time, and I watched some of his earliest procedures firsthand. I performed RK for a couple of years in my own practice, and for the past 27 years I have regularly looked after patients with RK-related problems. As a result, my perspective on the procedure has changed over the years.
PROBLEMS AFTER RK
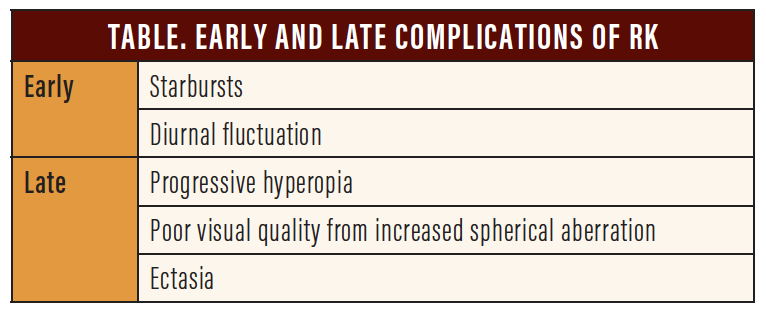
RK worked by essentially producing controlled ectasia in the periphery of the cornea. Because the cornea is an elastic dome, the periphery became elevated, and the central area flattened to produce the desired outcome of correcting myopia. Despite their positive effects, RK incisions cause several complications and side effects over time (Table). These include a progressive hyperopic shift, diurnal fluctuations in visual acuity, starbursts, ectasia, poor visual quality from increased spherical aberration, and rupture of the keratotomy scars if traumatized.
Shifts, fluctuations, and starbursts. In one study, 31% to 54% of patients developed progressive hyperopia 5 to 12 years after RK surgery as a result of continued peripheral corneal elevation and central flattening.1 In another study of RK eyes, mountaineers experienced a moderate hyperopic shift at high altitudes that returned to baseline on descent.2 The causes were determined to be relative hypoxia and a relative reduction in corneal metabolism because of the RK incisions.2,3
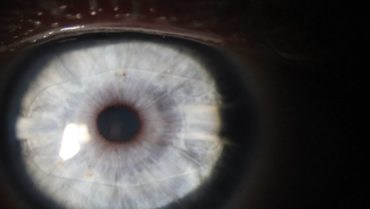
Ectasia. In some cases, particularly inferotemporal, RK incisions become more ectatic over time. This is often the case in eyes that have epithelial cysts or are originally predisposed to developing keratoconus, and ectasia is sometimes exacerbated by the performance of additional corneal ablative surgery for hyperopic correction. By ablating elevated areas, this secondary intervention steepens the cornea but also thins mechanically weak tissue, thereby contributing to ectatic progression (Figure 2).
Poor visual quality from increased spherical aberration. RK patients often report a deterioration in visual quality as they age. In most cases, these patients have developed spherical aberration in their crystalline lenses, which compounds the spherical aberration induced by RK.
MANAGEMENT STRATEGIES
Starbursts. The location of RK incisions in the pupillary zone can cause starbursts. The phenomenon is most evident at night when the pupil is dilated and when there are point sources of light. Most RK patients adapt to starbursts, but, if they find the condition debilitating, then prescribing brimonidine tartrate ophthalmic solution or low-dose pilocarpine to constrict the pupil may resolve the problem.
Progressive hyperopic shift. Perhaps the most common complication after RK, a progressive hyperopic shift is most often experienced by patients with symptoms of presbyopia. In addition to a loss of accommodation from presbyopia, patients have lost the mechanism previously used to compensate for their hyperopia and thus are unable to see well at distance and near.
Laser vision correction. The simplest option for most refractive surgeons, but likely not the best, is to perform laser vision correction (LASIK or PRK) to address the shift. I used this technique starting in 1993, but long-term I have found it only to cause more problems, including further hyperopic progression and ectasia (Figure 2).
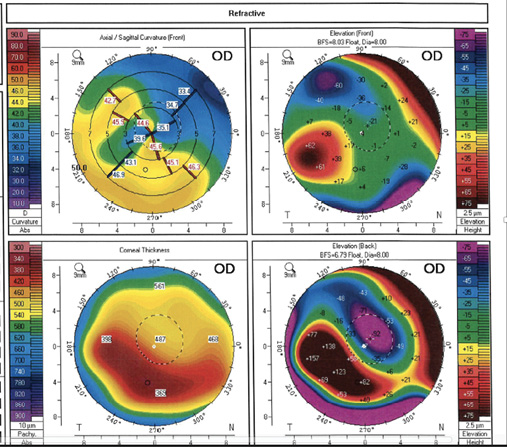
Figure 2. Keratoconus developed in this eye after laser ablation to correct a progressive hyperopic shift.
Some have described good short-term results after PRK with mitomycin C (MMC),4 but patients can develop severe haze caused by the activated keratocytes. The post-RK patient in Figure 3 developed haze after PRK with MMC. After a second PRK treatment with adjunctive MMC (Figure 3A), the patient developed more significant haze that persisted for more than 2 years. I used a microkeratome to perform a superficial homoplastic anterior lamellar keratoplasty, which removed the anterior cornea and replaced it with a free LASIK-type flap, resulting in restoration of the patient’s visual acuity and a reduction in starbursts (Figure 3B).
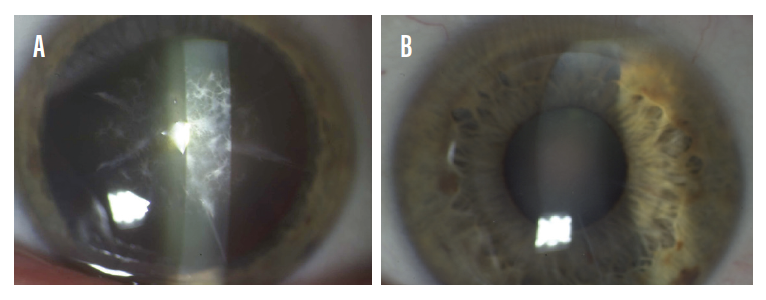
Figure 3. Repeat PRK with MMC was performed on this post-RK eye (A). A microkeratome superficial homoplastic anterior lamellar keratoplasty was performed to resolve the significant haze that developed (B).
Lasso stitch. Another option is the lasso stitch. There are two useful variations: the Grene lasso developed by R. Bruce Grene, MD, and the double lasso stitch. Either technique can be especially useful in patients with diurnal fluctuations in visual acuity. It can also slow or arrest progressive hyperopic change in the long term. In the Grene lasso technique, a Mersilene 10-0 nonelastic suture (polyethylene terephthalate; Ethicon) is placed through each RK incision at a 7-mm optic zone and tightened to achieve steepening that is double the intended amount. Patients are myopic initially. As the suture cheese-wires through the stroma, however, the cornea flattens, and the refraction heads toward emmetropia.
In the double-suture technique, two lasso sutures are fashioned at the 7- and 9-mm optical zones. Rather than pass the suture through the incisions, the surgeon passes the sutures through the stroma so that they lie over the incisions. Once the sutures cheese-wire into the midstroma, they provide a similar effect as a single lasso suture placed through the incisions. The overlay technique of the double lasso is technically easier to perform than the Grene lasso and produces a similar effect without disrupting the RK incisions (Figures 4A and 4B).
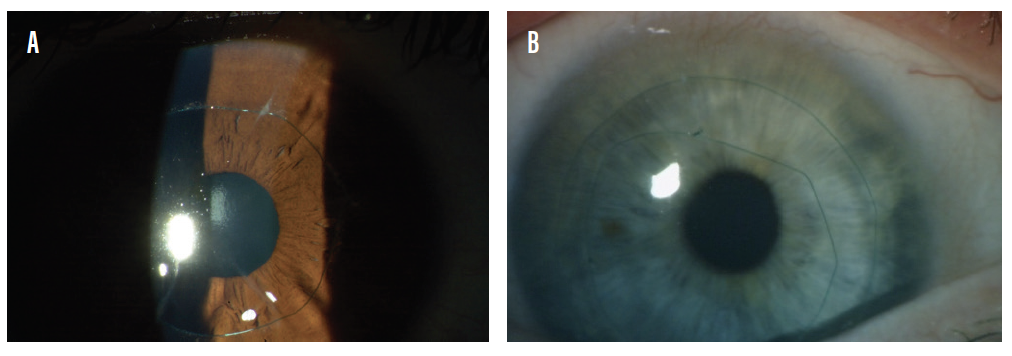
Figure 4. Single (A) and double (B) lasso sutures. In the single-suture technique, sutures are passed through the incisions; in the double-suture technique, the sutures are passed through the stroma so they lie over the incisions.
Phakic IOL implantation. A more accurate alternative compared to lasso suturing and laser ablation is implantation of a hyperopic phakic IOL (Figure 5) such as the Visian ICL (STAAR Surgical) or the Artisan/Verisyse (Ophtec/Johnson & Johnson Vision). An advantage of this approach is that the IOL can be removed or replaced later if need be.
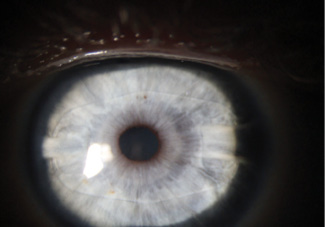
Figure 5. An Artisan IOL was implanted in this eye 10 years after RK to address a 3.50 D progressive hyperopic shift.
Cataract surgery or refractive lens exchange. Patients who have cataracts or who are of age for a refractive lens exchange can benefit from lensectomy and implantation of a small-aperture lens. The IC-8 IOL (AcuFocus; not approved by the FDA) can provide post-RK patients with increased depth of focus; I have found that the lens is also forgiving of astigmatism and eliminates starbursts. The patients in whom I have implanted the IC-8 bilaterally (Figure 6) have achieved spectacle independence. Piggybacking is an alternative: An XtraFocus M93L small-aperture IOL (Morcher; not approved by the FDA) is placed in the sulcus over a monofocal lens in the capsular bag.
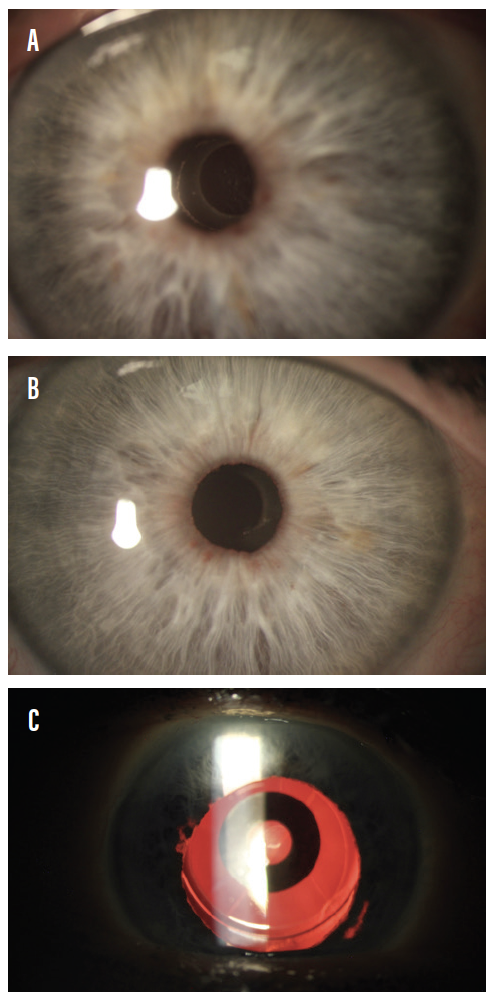
Figure 6. AcuFocus IC-8 IOLs were implanted bilaterally in a patient who had undergone RK. The edge of the small-aperture IOL can be seen within the pupil of the right eye (A). In the left eye (B), retroillimination reveals the IC-8 IOL and the RK incisions (C).
Meticulous surgical planning is important regardless of the approach to lens surgery, and IOL power calculations are challenging in RK patients. A variety of options are available, but my personal preference is to use the keratometry readings from the Holladay Report (Pentacam, Oculus Optikgeräte) and the Holladay 2 formula.
Placement of the incision to access the anterior chamber is also important. RK incisions are best avoided by performing a scleral incision. Alternatively, a limbal or corneal incision is best placed between the RK incisions and set as posteriorly as possible.
CONCLUSION
In the late 1980s, RK was considered to be a phenomenal procedure and the only option available to correct myopia. The drawbacks of RK became evident over time, and unhappy RK patients continue to present to ophthalmology practices periodically. An understanding of the procedure’s complications and options for their management can allow surgeons to help patients achieve better visual outcomes and improve their quality of life.
1. Deitz MR, Sanders DR, Raanan MG, DeLuca M. Long-term (5- to 12-year) follow-up of metal-blade radial keratotomy procedures. Arch Ophthalmol. 1994;112(5):614-620.
2. Ng JD, White LJ, Parmley VC, et al. Effects of simulated high altitude on patients who have had radial keratotomy. Ophthalmology. 1996;103(3):452-457.
3. Sanders DR, Deitz MR, Gallagher D. Factors affecting predictability of radial keratotomy. Ophthalmology. 1985;92(9):1237-1243.
4. Ghoreishi M, Abtahi AM, Seyedzadeh I, et al. Photorefractive keratectomy in the management of postradial keratotomy hyperopia and astigmatism. J Res Med Sci. 2017;22:82.