
Advances in femtosecond laser technology at the turn of 21st century helped to improve the precision and safety of LASIK. Further innovation in femtosecond technology with the introduction of the small-incision lenticule extraction (SMILE) technique marked another milestone in corneal refractive surgery. The biggest limiting factor with corneal refractive surgery now lies in the limitations of the cornea itself.
Today, the femtosecond laser is poised to carve out a new role for itself in IOL surgery. Experimental work by Sahler et al1 has shown that it is possible to create a negative refractive index change in a hydrophobic acrylic material by exposing the material to water and low energy light from a femtosecond laser at 520 nm wavelength. This approach, known as refractive index shaping, is an exciting new technology being developed by Perfect Lens. If the successful experimental results to date are carried forward into successful clinical trials, this technology may have the ability to change the power of an IOL after implantation to adjust sphere, toricity, or a combination of sphere and toricity—and even to add or remove multifocality. This last capability would give practitioners the ability to eliminate the unwanted dysphotopsias that some patients experience with multifocal IOLs.
FIXING REFRACTIVE SURPRISES
In the event of residual refractive error or postoperative refractive surprise after IOL implantation, the refractive index shaping device could be used to change the IOL power to correct the refractive error postoperatively. This technology could minimize the need for lens explantation or additional touchup corneal refractive procedures due to unsatisfactory refractive results of cataract surgery.
Power changes of up to 4.00 D have been successfully accomplished in bench testing and animal studies. The technology could also potentially be used in complex cases to treat limited amounts of higher-order aberrations.
The treatment area is a disc-shaped segment within the IOL optic with a diameter of at least 4 mm and depth of 50 µm. Treatment algorithms direct the laser via scanning movements to create a disc of refractive index gradation to modify up to 4.00 D of positive or negative sphere and 3.00 D of astigmatism (Figure). A rabbit study showed an average of 3.60 D change could be achieved with error of less than 0.10 D and standard deviation of 0.03 D.2 Another experimental study found that the technology could be used to accurately adjust dioptric power in a commercially available hydrophobic acrylic IOL without significantly altering the qualities of the IOL, including modulation transfer function, light transmission, and light scattering.3
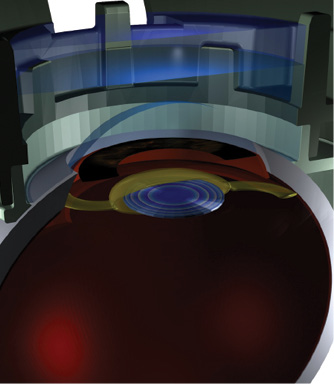
Figure. Artist’s conception of femtosecond laser treatment done on an IOL to change its refractive index and correct postoperative refractive error.
WIDELY APPLICABLE
This approach to postoperative power adjustment has potential advantages over other IOL power-adjustable technologies because it could be applied to many commercially available acrylic IOLs. Additionally, it does not depend on a special IOL material, and there would be no time restrictions regarding when it can be done postoperatively. It would be a minimally invasive laser treatment that potentially could be performed in a doctor’s office under topical anesthesia.
The ability to customize spherocylindrical treatment and to place or remove multifocality would create a paradigm shift in how surgeons address their patients’ lens choices. True customization of refractive outcomes with IOL technology could be achieved. Wound healing and corneal limitations might no longer be a factor in the postoperative adjustment of refractive errors. This would give patients a true choice of customization and surgeons a tool to correct potentially unwanted visual side effects that patients cannot neurally adapt to with no time period limitation.
In vivo clinical studies of the Perfect Lens are under way.
1. Sahler R, Bille J, Sean E, Chhoeung S, Chan K. Creation of a refractive lens within an existing intraocular lens using a femtosecond laser. J Cataract Refract Surg. 2016;42(8):1207-1215.
2. Werner L, Ludlow J, Nguyen J, et al. Biocompatibility of intraocular lens power adjustment using a femtosecond laser in a rabbit model. J Cataract Refract Surg. 2017;43(8):1100-1106.
3. Nguyen J, Werner L, Ludlow J, et al. Intraocular lens power adjustment by a femtosecond laser: In vitro evaluation of power change, modulation transfer function, light transmission, and light scattering in a blue light-filtering lens. J Cataract Refract Surg. 2018;44(2):226-230.


