
Raindrop (ReVision Optics, Inc.) is an inlay that reshapes the cornea to improve near vision. Approved for treatment of emmetropic presbyopes with refractions from -0.50 D to +1.00 D (≤ 0.75 D cyl), Raindrop helps patients aged 41 to 65 greatly reduce or, in some cases, eliminate their need for reading glasses. Since the technology was FDA approved in 2016, more than 2,500 patients have received the inlay from the 130-plus surgeons performing the procedure in the United States.1
As a surgeon, it was always a disappointment that we could not offer the same level of treatment to presbyopic patients that we give to patients with other refractive problems. The only ways to treat presbyopia were glasses, multifocal or monovision contact lenses, monovision LASIK, and clear lens extraction (CLE) with monovision or multifocal IOLs. Because only about half of all presbyopes will tolerate true monovision, and many did not like multifocal contacts, many patients were encouraged to wait on newer technologies down the road.
Now that technology is here. Raindrop improves near vision by 5 lines and intermediate vision by 2.5 lines.2 Finally, we can help patients reduce or eliminate their need for reading glasses.
Raindrop Procedure and Outcomes
The Raindrop procedure is very straightforward and relies on our existing skills. The surgeon makes a flap using a femtosecond laser at 30% of the corneal thickness, somewhat deeper than a standard LASIK flap. The technique used to deliver and center the inlay is very user friendly.
To place the inlay, the Raindrop delivery device is placed in contact with the cornea stromal bed centrally over the pupil with the flap reflected. A Barraquer spatula or other instrument is used to stabilize the inlay on the stroma while the surgeon slides away the delivery device. The inlay can then be centered on the light-constricted pupil by gently nudging it with the elbow of the instrument. Once in position, the inlay is allowed to dry for approximately 1 minute and adhere to the stroma. The corneal flap is then replaced.
I have performed about 50 Raindrop procedures, and the outcomes have been excellent. Patients have good near and intermediate vision, and bilateral distance vision is preserved. Raindrop is placed in the non-dominant eye, and the dominant eye becomes the workhorse for distance vision, so if a patient’s distance vision is not perfect, I also perform LASIK on the dominant eye.
Raindrop Registry
In the Raindrop Registry, practices can record their outcomes and compare them against national data. The registry gives surgeons a dashboard view of the visual acuities they have achieved and details about their procedure, as well as patients’ satisfaction and spectacle independence at near. Today, over 1,170 patients from more than 90 practices are in the registry, including mine.
Among patients in the registry, UNVA in the treated eye is 20/25 or better for 62% of patients and 20/40 or better for 89%. UDVA in the treated eye is 86% 20/25 or better and 95% at or above 20/40 (Figure 1).2 About 76% of patients never used spectacles and 18% sometimes wore spectacles, and patient satisfaction is 88% based upon their last available visit (Figure 2).2
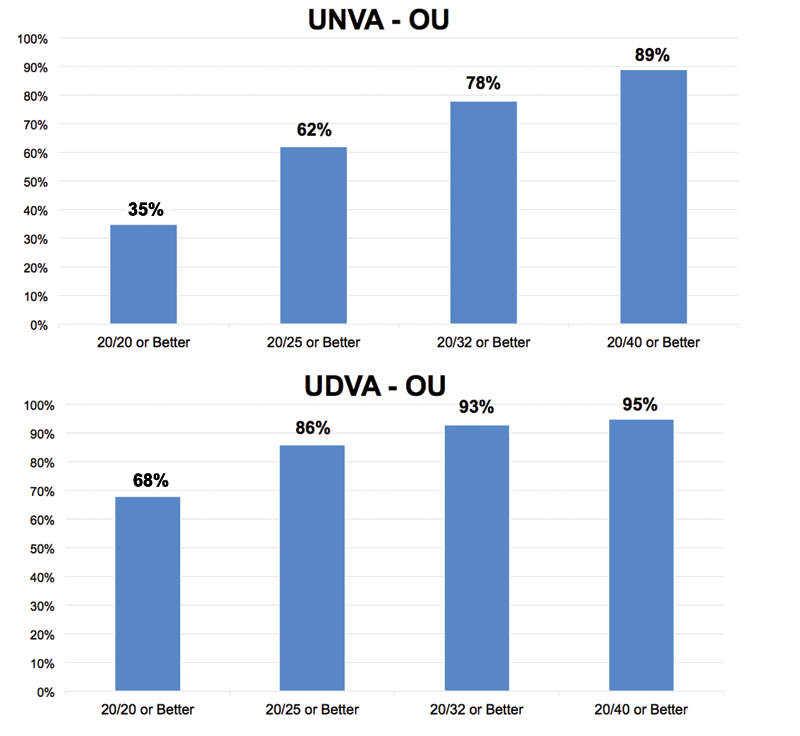
Figure 1. Visual acuities from the Raindrop Registry.

Figure 2. Patient feedback from the Raindrop Registry.
Workflow
Based on the patient check-in questionnaire, technicians capture preoperative measurements for Raindrop before I see the patient. Tests are the same as LASIK: corneal topography, corneal tomography, and optical or ultrasound pachymetry, as well as evaluation for dry eye including tear osmolarity and meibography. When I see the patients, they need a good slit-lamp examination to assess the cornea, crystalline lens, and tear film.
On surgery days, the Raindrop workflow is typical of LASIK, so it fits right in with our normal workflow. It takes 1 to 2 minutes to deliver and position the inlay with an overall surgery time of less than 10 minutes. After the patient goes to recovery with the inlay in a good position as expected, we spend a little more time counseling them about postoperative care. Raindrop patients need to use drops for a longer period than LASIK patients. Although the hydrogel material is very biocompatible, a very small percentage of patients (approximately 4% of the surgical subgroup in the FDA study) may want or need removal of the inlay, and this risk is increased if patients do not use their drops as instructed.3 Patients take an antibiotic drop for 1 week, plus difluprednol (Durezol; Novartis), a potent steroid drop, for the first month on a 4-3-2-1 taper, followed by loteprednol (Lotemax; Bausch + Lomb), a milder steroid, twice a day in the second month, and then once a day in the third month.
Discussion With Patients
When I discuss Raindrop with my patients, I tell them that I cannot make them 20 years old again. No solution will restore the eye’s natural autofocus. The Raindrop, however, changes the cornea to improve near vision without glasses.
Safety is a very important part of the discussion. Raindrop is removable, so in the rare case that a patient does not like it, I can remove it and they will revert to their pre-surgery vision. I tell patients that the Raindrop material has been used for many years in contact lenses and lens implants, and the only difference is that we are placing it in the cornea. The Raindrop procedure also preserves the crystalline lens, which allows them to postpone cataract surgery if the lens is in good shape.
Finally, expectations are key. When patients who have Raindrop are reading very fine text for a long period or reading in low light, they may feel more comfortable with low-powered reading glasses.
There is an umbrella effect among people who want to read more clearly as well, because some patients who inquire about Raindrop have problems that can be resolved with cataract surgery or LASIK. In a survey by ReVision Optics of surgeons using Raindrop, 60% noted an increase in CLE/cataract procedures, and 58% saw more LASIK cases.4 This technology that fills a need for so many of our patients also helps build the practice.
To see videos of a Raindrop procedure, go to bit.ly/2i9dXPe
1. ReVision Optics data on file, 2017.
2. Raindrop Registry data on file, 2017.
3. Raindrop Near Vision Inlay Professional Use Information. ReVision Optics. March 2017. https://www.accessdata.fda.gov/cdrh_docs/pdf15/p150034c.pdf. Accessed November 27, 2017.
4. ReVision Optics. Survey of Raindrop users performed via Survey Monkey. November 2017.
