
Sustainability of natural resources and reduction of waste are growing imperatives as concerns about climate change mount.1 United Nations Secretary-General António Guterres recently called climate change “the most systemic threat to humankind” and urged world leaders to curb their countries’ greenhouse gas emissions.2
The provision of health care is increasingly recognized as a significant source of greenhouse gas emissions and other pollutants, and subsequently efforts are on the rise to improve the environmental performance of health care delivery and reduce its carbon footprint.
Hospitals have been identified as among the most energy-intensive commercial buildings in the United States,3 and efforts to go green by modernizing their heating and cooling systems are increasingly in the news. Further, ORs generate 20% to 33% of total hospital waste, and management of medical waste carries significant environmental and financial costs.4-6
Cassandra Thiel, PhD, a public health researcher and assistant professor in New York University’s department of population health, told CRST that, “as health care systems and professionals worldwide become more aware of and concerned for the public health implications of climate change and excessive resource use, efficient care delivery models must be better understood and promoted.”
CATARACT SURGERY’S CARBON FOOTPRINT
As the most commonly performed surgical procedure worldwide, cataract surgery contributes significantly to the carbon footprint of the health care facilities where it is performed.7 The term carbon footprint is generally used to refer to greenhouse gas emissions resulting from the full life cycle of a product or process. The carbon footprint of a single phacoemulsification episode has been estimated to be comparable to that of a typical person’s life for an entire week.8
Dr. Thiel has published extensively on the environmental impact of surgical procedures.9-12 Most recently, she and her colleagues looked at the environmental impact of phacoemulsification in the United States.13 Their study of the life-cycle emissions and environmental impact of materials used to perform phacoemulsification at four US surgery centers revealed that the carbon footprint of surgical materials from phacoemulsification (excluding drugs and the phaco unit itself) averaged 35 kg of carbon dioxide equivalent (kg-CO2eq) of greenhouse gas emissions—that’s the same quantity of emissions associated with driving a car about 85 miles.
Single-use disposable materials, such as drapes and basins, accounted for 83% of those emissions, with 80% originating in the production of those items and 20% in their disposal. Reusable instruments, such as forceps and scissors, accounted for an average of 6 kg-CO2eq of greenhouse gas emissions, 70% of which was associated with sterilization.
“With increasing concerns for the health implications of climate change and environmental degradation, we need to reexamine our policies on single-use and disposable materials,” Dr. Thiel concluded. Through evidence-based practice, she said, “we can minimize the footprint of ophthalmic surgeries and optimize our resource and financial efficiency in the operating room.”
MODEL OF EFFICIENCY
Dr. Thiel points to Aravind Eye Care System in India as a model of energy efficiency (see Aravind’s Initiatives). Aravind, whose surgeons perform 750 to 1,500 cataract procedures per day, has instituted numerous processes that dramatically reduce its carbon footprint. The processes originated in an attempt to optimize efficiency, productivity, and resource utilization, and have culminated in a reduction in greenhouse gas emissions. Natarajan Vengadesan, manager of quality and patient safety at the Aravind Eye Hospital facility in Pondicherry, India, told CRST that, after the processes were implemented, “it became apparent that those processes had a major impact on the environment, so increased effort was devoted to identifying additional opportunities for sustainable initiatives that would benefit the organization, as well as the environment.”
Aravind’s Initiatives
Aravind Eye Hospital’s Pondicherry facility, spread over 20 acres, has a 700-bed capacity. The facility has made remarkable progress reducing its carbon footprint through a variety of means. Natarajan Vengadesan, manager of quality and patient safety for Aravind Eye Hospital, shared the following specifics about what makes Aravind Pondicherry a model of efficiency for other hospitals:
- India is a tropical country; there is much sunshine, and it is effectively used. Building construction allows a maximum amount of natural light to enter, and all lighting has been upgraded to LED.
- Only patient-care areas and other key areas have air conditioning. All the air conditioning units have been fixed with regulators, and timing units have been installed in all cooling units to minimize usage.
- For alternative energy generation, a solar plant has been installed. This reduces CO2 emission by about 200,000 kg per year.
- Examination and surgical procedures are completed on the same day to minimize patient visits and therefore travel. Primary eye care centers provide transport to outreach camps; this has reduced patient travel. Also, Aravind provides staff quarters and a nursing hostel within the hospital campus; more than 90% of the total 650 staff live there and walk to the hospital.
- Through its high surgical productivity and resource utilization system, Aravind generates just 0.25 kg of waste per surgery, compared to the United States, where 2.25 kg of waste is generated per surgery.
- Waterless urinals have been installed; this saves about 90% of water use. A rainwater harvesting soak pit recharges the ground water. Southeast Asia’s largest waste water treatment plant, using decentralized waste water treatment system technology, is able to treat 100 m3 out of 120 m3 of waste water.
Alan L. Robin, MD, has had a decades-long relationship with Aravind. He helped establish its glaucoma department and has witnessed the evolution of the health care system there. He has seen its development from predominantly a charitable organization dedicated to preventing blindness in earlier days to its current status as a role model for hospitals around the world interested in quality and efficiency in the delivery of eye health care.
Dr. Robin noted that, although restrictive regulations in developed countries often make it difficult to implement innovative processes aimed at minimizing waste, Aravind and other eye care facilities in India are not hampered by such constraints. He cited the requirement that US eye surgeons don a new disposable mask for each case and the prohibition against using dilating drops from one bottle for more than one cataract patient—practices that result in significant waste of disposables, eye drops, and their containers.
“When data show that changes will reduce waste and increase energy efficiency, Aravind can implement those changes,” he said. “In the United States, we have to dispose of the mostly full eye drop bottle or send it home with the patient.” Either way, he suggested, the practice adds to the cost of surgery and increases the amount of glass and plastic in the trash stream. Dr. Robin is an outspoken critic of regulations that lead to waste, which, he said, “represents a threat to society.” He suggested that, if the US health care system were less encumbered, some of the energy-saving processes employed by Aravind could be implemented here.
“If we don’t think about the future and try to cut down the costs of health care sensibly and get rid of needless regulations that often are of no benefit,” he warned, “then we will ultimately cause great harm to our children, our children’s children, and their children.”
Until a few years ago, the environmental impact of Aravind’s waste reduction efforts had not been quantified, said Rengaraj Venkatesh, MD, chief medical officer of Aravind’s Pondicherry facility. Dr. Robin brought Aravind’s work to the attention of Dr. Thiel, and a study was planned. From November 2014 through February 2015, Dr. Thiel analyzed Aravind’s surgical materials, energy use, and waste from cataract surgery, and calculated the resulting greenhouse gas emissions and the emissions related to ozone depletion, water eutrophication, toxicity, and air pollution. She found that Aravind generated 250 g of waste per phaco procedure and nearly 6 kg-CO2eq, which is 5% of the carbon footprint of phacoemulsification in the United Kingdom with comparable or better outcomes. She estimated that the difference in phaco energy expenditure between Aravind and the United States would be as great, if not greater.14
In the report of their findings, Dr. Thiel’s team explained that the emissions associated with a phaco procedure at Aravind were comparable to those of a car driven 14 miles, whereas emissions from a similar procedure in the United Kingdom were comparable to those of a car driven 391 miles. Practices at Aravind that made the most difference were shorter surgery duration; reuse of surgical gowns, caps, booties, and blankets; use of multiuse pharmaceuticals; and more efficient sterilization of stainless steel instruments, so that they can be reused the same day.14
“Our overuse of disposable materials in surgery in the United States is unsustainable,” Dr. Thiel told CRST. “Ophthalmologists and other medical specialists should seek ways to reduce material use and emissions in medical procedures. This center in India can serve as a model.”
LESSONS LEARNED
Aravind’s advances in energy efficiency are taking place concomitantly with an effort in India to end preventable blindness (a goal of the World Health Organization’s Vision 2020 initiative) by doubling the current rate of cataract surgery.15-18 If India’s ophthalmologists used the surgical methods currently used in the United Kingdom to achieve that goal, they would emit the same amount of greenhouse gases as a year’s driving of 250,000 passenger vehicles, Dr. Thiel and colleagues estimated. By contrast, if all of India’s eye care facilities employed Aravind’s approach, they would emit the greenhouse gases equivalent to only 9,000 passenger vehicles' yearly emissions (www.youtube.com/watch?v=OArrvXqV43Y).14
“Aravind demonstrates that reusable surgical materials can produce excellent patient outcomes while reducing costs and lessening the environmental footprint,” she said (see Sustainability and Safety).
SUSTAINABILITY AND SAFETY
Although regulations may slow the path toward waste reduction, they do so at least theoretically in the interest of patient safety. Two studies reached differing conclusions on safety issues with reuse of phaco tips, which is one potential area of savings and waste reduction.
Cecchini et al compared unused phaco tips with tips after a single use and with tips after multiple uses.1 They found that the used tips showed relevant signs of deterioration and deposition of biologic material, mostly involving the outer edge. They concluded that the adoption of single-use, disposable phaco tips seems to be highly advisable.
Tsaousis et al performed a laboratory study evaluating morphologic changes after multiple uses of different types of phaco tips in an ex vivo model.2 They found that ex vivo experimental simulations of heavy clinical reuse did not result in significant ultrastructural damage to the phaco tips. Additionally, when the tips were subjected to identical experimental conditions in reuse, there was no ultrastructural difference in the durability or integrity of the phaco tips that were labeled for single use or for multiple uses.
These authors stated that the recommendation to adopt only single-use disposable phaco tips did not appear to be based on meaningful clinical evidence.
“In some settings, such as in US regulatory agencies, they might insist on strict adherence to manufacturer instructions for use. However, it is not clear whether all recommendations contained in the instructions for use are based on rigorous scientific testing,” these authors concluded. “It appears that labeling some titanium phaco tips for single use is rather arbitrary, in particular when another manufacturer labels a similar tip for up to 50 uses. That the same manufacturer labels some tips single use and other ultrastructurally identical tips for up to 20 uses suggests that there is no scientific basis for prohibiting reuse of the single-use tip. We therefore recommend that cataract surgeons be allowed discretion in terms of reusing phaco tips based on their best clinical observations and judgment. This could ultimately help reduce the seemingly unnecessary higher costs associated with single-use phaco tips.”
1. Cecchini, P, D’Aloisio, R, Antonuccio, et al. Chemical and physical analysis of phaco tips surface before and after cataract surgery. J Cataract Refract Surg. 2017;43:1107-1114.
2. Tsaousis, KT, Chang, DF, Werner L, et al. Comparison of different types of phacoemulsification tips. III. Morphological changes induced after multiple uses in an ex vivo model. J Cataract Refract Surg. 2018; 44(1):91-97.
Although the study of cataract surgery's carbon footprint aimed to identify ways to be more efficient by evaluating how much waste was generated from surgery, Dr. Venkatesh and his colleagues learned that the health system’s carbon footprint is related to many more variables beyond waste, he explained.
“For instance, we learned that travel adds considerably to Aravind’s carbon footprint,” he said. “And, although we have been active in patient outreach, bringing patients in groups to the hospital for cataract surgery and returning them as a group, for over 40 years, we realized that there is a lot more we could do. We now proactively encourage follow-up at our centralized vision centers for postoperative patients who walk to the base hospital for treatment.”
Efforts throughout Aravind are being made to allow patients to complete the entire patient care loop in a single visit, from diagnosis through interpretation and intervention, Thulasiraj D. Ravilla, executive director of Lions Aravind Institute of Community Ophthalmology (LAICO), the training and consulting arm of the Aravind Eye Care System, told CRST. “There are places where it takes three or four visits for a patient to get a pair of glasses, and elsewhere it definitely takes three or four visits for cataract surgery. By reducing this to one visit for all patients, it will have a tremendous impact on our carbon footprint, but also on other things. For instance, it is more patient-friendly, and it is more cost-efficient for the patients and more efficient overall for the hospital. Now we are trying to spread awareness to practitioners outside of the Aravind System so that we can help influence process improvements on a national level.”
SPREADING THE MODEL
Dr. Venkatesh said lessons from Aravind could be applied in the United States, Europe, and other developed countries if regulatory restrictions could be overcome.
“Regulations that are more stringent are the only thing preventing hospitals from implementing the systems that have increased our productivity, cost-efficiency, and environmental success,” he said. “We consider quality as the driver for all our initiatives; we in no way would compromise on quality. That being said, we can use reuse items that would not be possible to reuse in countries like the United States.”
Dr. Thiel noted that most of Aravind’s environmental initiatives were probably initially implemented in the name of cost savings or increasing throughput, and these goals are not mutually exclusive. “Hospitals and medical facilities are starting to enact measures to reduce their environmental footprint, but they will always analyze life-cycle costs to be sure the initiative is sustainable from multiple perspectives,” she said.
Some US eye care facilities are taking steps to decrease their carbon footprints.Matthew P. Jensen, CEO of Vance Thompson Vision, in Sioux Falls, South Dakota, explained that the center is exploring the environmental benefits of reducing the number of visits that patients must make to the office. As the Aravind personnel have recognized, less travel means less travel-related greenhouse gas emissions.
Randall J. Olson, MD, CEO, of the John A. Moran Eye Institute in Salt Lake City, Utah, explained that his facility has partnered with the Aravind system in an effort to evaluate and possibly improve his facility's environmental behavior. “We have found that one reason our emissions are so much greater than Aravind’s is due to regulations that tend to give us little flexibility,” Dr. Olson said.
Despite those regulatory restrictions, Jeff Pettey, MD, vice chair for education at the Moran Eye Center, is working on a waste-reduction beta project. Following the lead of his colleague Alan S. Crandall, MD, he and a few other Moran staffers have begun bagging and disposing of what might be called clean waste from the OR. (Dr. Crandall started the recycling project after visiting Aravind.)
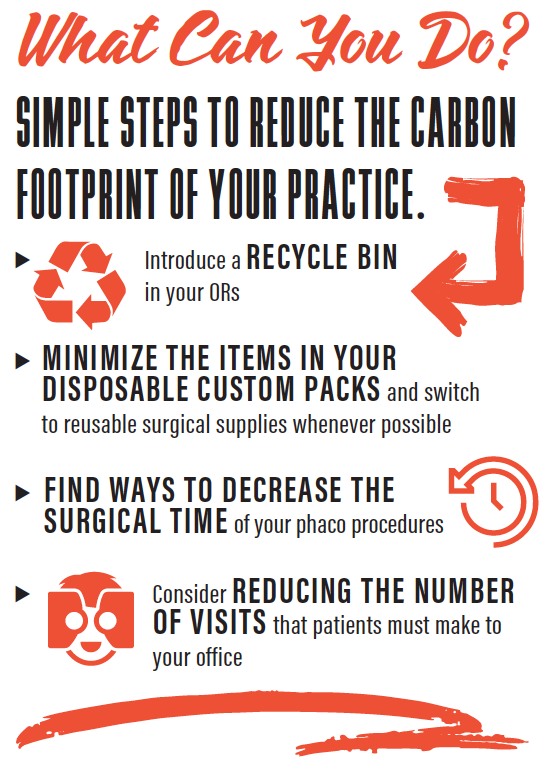
“There is so much paper and plastic from all of the packs we open for each procedure,” Dr. Pettey said. “Each surgery generates at least one large garbage bag of waste, and we’ve been taking the bags home to our recycle bins or to other available recycle repositories as sort of a beta project.” So far, he said, the project has required only a single extra trash bin in the OR.
“We just look through quickly at the end of the cases, and the refuse goes in the refuse bin and the recyclables go into the recycle bin,” he said. “Something we have learned over time is that if recycling is easy everyone will do it, but when it’s not convenient it doesn’t get done. So, just by introducing that extra recycle bin, this could be implemented in any OR without a whole lot of fanfare.”
The next phase, he said, is to expand the project throughout Moran. An OR group meeting is scheduled to evaluate that possibility. “It will take a commitment from the institution, and there may be a cost associated with doing this on a larger scale, but it is the next step that needs to be done,” he said.
Dr. Pettey said efforts to reduce waste by cutting down on disposal of instruments after a single use are laudable, but they face challenges. “There is a push toward single-use instruments in the United States due to sterilization concerns,” he said. “But we can’t overlook the fact that, by doing this, we are dramatically increasing not only the quantity of waste with those disposables, but also taking reusable instruments that could be used for hundreds or thousands of surgeries and doing away with them and ultimately just throwing them away.”
MAKING PROGRESS
Regulations notwithstanding, some surgical efficiencies are popping up in the US cataract surgery landscape. For instance, shorter surgery times are made possible in facilities where two ORs run simultaneously, and some hospitals and surgery centers have minimized the items in their disposable custom packs and switched to reusable surgical supplies.19
In their examination into cataract surgery and environmental sustainability, Dr. Thiel and colleagues discussed barriers that stymie environmental progress. “Although most regulations in developed countries are made with patient safety in mind, greater liability in countries such as the United States might drive resource use in operating rooms. Defensive medicine not based on scientific evidence of infectious risk adds to the cost and, therefore, the environmental footprint of care,”14 they wrote.
1. Honigsbaum M. Anthony Costello: making climate change part of health. Lancet. 2009;373(9676):1669.
2. Sengupta S. Biggest threat to humanity? Climate change, UN chief says. New York Times. March 29, 2018. https://www.nytimes.com/2018/03/29/climate/united-nations-climate-change.html. Accessed July 13, 2018.
3. Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PLoS One. 2016;11(6):e0157014.
4. Goldberg ME, Vekeman D, Torjman MC, Seltzer JL, Kynes T. Medical waste in the environment: Do anesthesia personnel have a role to play? J Clin Anesth. 1996;8(6):475-479.
5. Tieszen ME, Gruenberg JC. A quantitative, qualitative, and critical assessment of surgical waste. Surgeons venture through the trash can. JAMA. 1992;267(20):2765-2768.
6. Esaki, RK, Macario M. Wastage of supplies and drugs in the operating room. Medscape. October 21, 2009. https://www.medscape.com/viewarticle/710513. Accessed July 13, 2018.
7. Morris DS, Wright T, Somner JEA, et al. The carbon footprint of cataract surgery. Eye. 2013;27:495-501.
8. Venkatesh R, van Landingham SW, Khodifad AM, et al. Carbon footprint and cost-effectiveness of cataract surgery. Curr Opin Ophthalmol. 2016;27(1):82-88.
9. Thiel C, Duncan P, Woods N. Attitude of US obstetricians and gynaecologists to global warming and medical waste. J Health Serv Res Policy. 2017;22(3):162-167.
10. Unger SL, Hottle TA, Hobbs SR, et al. Do single use medical, devices containing biopolymers reduce the environmental impacts of surgical procedures compared with their plastic equivalents? J Health Serv Res Policy. 2017;22(4):218-225.
11. Campion N, Thiel C, Woods N, et al. Environmental life-cycle impacts of surgical material supply: a comparative LCA of disposable custom packs. Journal of Cleaner Production. 2005;94:46-55.
12. Thiel C, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the US. Environ Sci Technol. 2015;49(3):1779-1786.
13. Thiel C, Venkatesh R, Ravindran RD, et al. Eye on emissions: carbon footprint of cataract surgery in Aravind Eye Hospital. Film presented at: American Society of Cataract and Refractive Surgery Annual Meeting; May 6-10, 2016; New Orleans.
14. Thiel CL, Schehlein E, Ravilla T, et al. Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43(11):1391-1398.
15. International Agency for the Prevention of Blindness. Vision 2020 Action Plan 2006-2011. https://www.iapb.org/resources/vision-2020-action-plan-2006-2011/. Accessed July 13, 2018.
16. McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. 2006;367:859-869.
17. Murthy GVS, Gupta SK, John N, et al. Current status of cataract blindness and vision 2020: the right to sight initiative in India. Indian J Ophthalmol. 2008;56:489-494.
18. Foster A. Cataract and Vision 2020—the right to sight initiative. Br J Ophthalmol. 2001;85:635-637.
19. Campion N, Thiel CL, Woods NC, et al. Sustainable healthcare and environmental life-cycle impacts of disposable supplies: a focus on disposable custom packs. Journal of Cleaner Production. 2015;94:46-55.












