

Patients’ expectations of refractive cataract surgery are higher than ever. Those who pay for premium lenses demand less than 0.50 D of astigmatism, and those who choose a toric lens or arcuate incision are likely to expect even less residual cylinder.
Most toric nomograms require a number to be entered for surgically induced astigmatism (SIA), but determining one’s personal SIA can be time consuming. Often, trainees and young surgeons will enter an arbitrary number such 0.25 D. In addition, several sources recommend making the incision on the steep axis to alleviate cylinder. The good news is, now that cataract surgery incisions are smaller, cases are shorter, and nomograms are improved, SIA may not affect visual outcomes as much as it used to.
AT A GLANCE
- Now that cataract incisions are smaller, cases are shorter, and nomograms are improved, surgically induced astigmatism (SIA) may not affect outcomes as much as it used to.
- Several studies have shown that SIA decreases as the incision’s size decreases and that it can be further minimized by placing wounds temporally.
- To improve outcomes, surgeons should focus less on SIA and more on preoperative testing, the posterior cornea, IOL tilt, and effective lens position.
FACTORS IN SIA
SIA has always been an important factor in astigmatism management, because the incision causes flattening. The amount of SIA is related to the type, length, and location of the incision as well as the wound closure technique (Figure). Several studies have shown that SIA decreases as the wound’s size decreases (Table).1-6 One study showed a reduction in SIA from a 3-mm to a 2.6-mm incision and further reduction when the incision measured 2.2 mm at 90 days.1
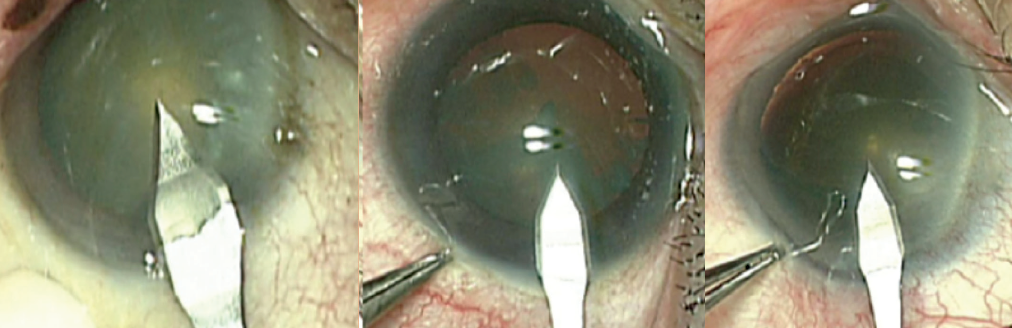
Figure. Comparison of 2.65-, 2.4-, and 2.2-mm cataract incisions.
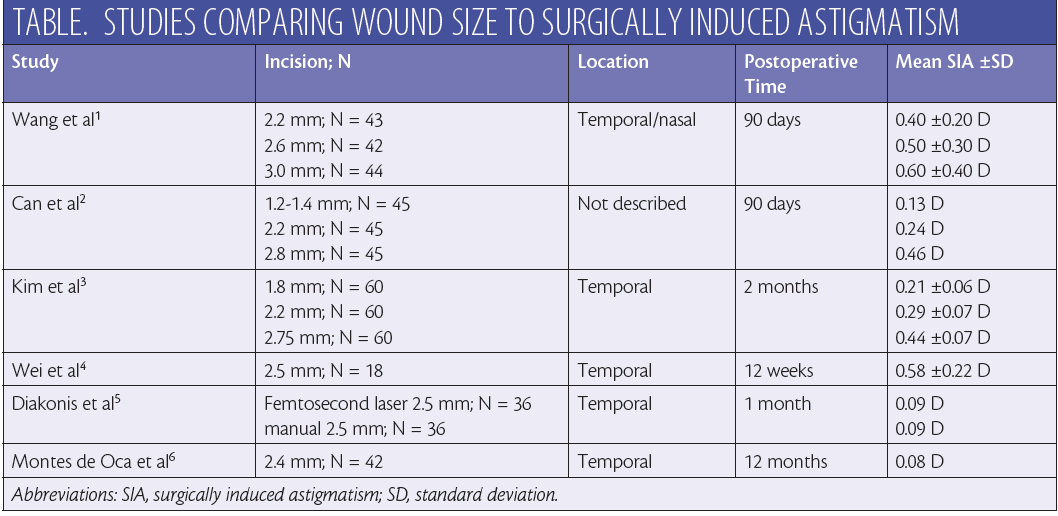
In addition, it matters when SIA is measured, because the wound stabilizes over the weeks following surgery. Diakonis et al showed that, at 1 month, the SIA was 0.09 D for a temporal 2.5-mm manual incision and for laser incisions of the same size.5 Our study showed similar SIA results at 1 year with a 2.4-mm temporal incision.6
EXCEPTIONS
Outliers always exist, and some corneas may react differently to the creation of a wound. The incision’s location can also make a difference. Wounds that involve the nasal or the superior nasal quadrant can cause higher SIA and more variability than temporal wounds.7
Eyes with keratoconus and postgraft eyes often overcorrect when a surgeon creates an astigmatic keratometry incision, so they may also develop unusual astigmatism from cataract incisions.8 Furthermore, factors outside of the actual incision’s creation, such as manipulation of the wound during surgery, may increase the severity of SIA.
SUMMARY
Most SIA is minimal when the surgeon uses a temporal 2.2- to 2.4-mm cataract incision. Creating the wound in the steep axis will seldom assist in clinically significant flattening, so surgeons should operate where they feel the most comfortable. SIA is minor when compared to other causes of unanticipated residual astigmatism such as ocular surface issues, variable preoperative testing, posterior corneal astigmatism, IOL tilt, and effective lens position. Rather than specifically study SIA, newer surgeons should focus on these other factors in astigmatism management to improve outcomes.
1. Wang J, Zhang EK, Fan WY, et al. The effect of micro-incision and small-incision coaxial phaco-emulsification on corneal astigmatism. Clin Exp Ophthalmol. 2009;37(7):664-669.
2. Can I, Takmaz T, Yildiz Y, et al. Coaxial, microcoaxial, and biaxial microincision cataract surgery: prospective comparative study. J Cataract Refract Surg. 2010;36(5):740-746.
3. Kim EC, Byun YS, Kim MS. Microincision versus small-incision coaxial cataract surgery using different power modes for hard nuclear cataract. J Cataract Refract Surg. 2011;37(10):1799-1805.
4. Wei YH, Chen WL, Su PY, et al. The influence of corneal wound size on surgically induced corneal astigmatism after phacoemulsification. J Formos Med Assoc. 2012;111(5):284-289.
5. Diakonis VF, Yesilirmak N, Cabot F, et al. Comparison of surgically induced astigmatism between femtosecond laser and manual clear corneal incisions for cataract surgery. J Cataract Refract Surg. 2015;41(10):2075-2080.
6. Montes de Oca I, Khandelwal SS, Al-Mohtaseb Z, et al. Long-term surgically induced astigmatism after cataract surgery. Paper presented at: American Society of Cataract and Refractive Surgery Annual Meeting. May 6-10, 2016; New Orleans, LA.
7. Barequet IS, Yu E, Vitale S, et al. Astigmatism outcomes of horizontal temporal versus nasal clear corneal incision cataract surgery. J Cataract Refract Surg. 2004;30(2):418-423.
8. Kubaloglu A, Coskun E, Sari ES, et al. Comparison of astigmatic keratotomy results in deep anterior lamellar keratoplasty and penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2011;151(4):637-643.




