The introduction of femtosecond lasers and their ability to create precise, reliable incisions enables me to deliver superior outcomes compared with toric lenses in patients with low to moderate corneal cylinder. This article offers my suggestions on how to continually improve the practice of laser cataract surgery.
SELECT THE RIGHT PATIENTS
Successful astigmatic correction starts with patient selection. The preoperative consultation period is the perfect time to raise the subject of correcting astigmatism with a laser. In my patient population, the mean preoperative cylinder is about 1.00 D. In my hands, astigmatic incisions provide excellent visual outcomes for up to 1.50 D of against-the-rule and up to 1.75 D of with-the-rule astigmatism. For surgeons new to laser astigmatic incisions, I recommend choosing patients with lower amounts of cylinder in a tighter range: 0.75 to 1.25 D. Treating this level of cylinder has a high impact, and the nomogram is easily titrated. After perfecting his or her outcomes in this range, the surgeon can expand into lower and higher levels of astigmatism.
AT A GLANCE
- Patient selection is important to the overall success of laser cataract surgery. Surgeons who are new to laser cataract surgery should start with patients who have 0.75 to 1.25 D of cylinder. More experienced surgeons can successfully treat a broader range.
- The ideal candidate is one who understands what laser cataract surgery is and the value it can provide. Incorporating video education elements and written materials into the consultations reinforces the messaging.
- It is important to control for variables to improve outcomes. The author credits Six Sigma lean processes and her femtosecond laser for her successful outcomes. Her mean postoperative refractive cylinder at 3 months is 0.17 D, with 82% of patients with less than 0.25 D of astigmatism and 95% of patients with less than 0.50 D of astigmatism.
It is important to set patients’ expectations during the initial consultation and to clarify that the goal is to reduce, not necessarily eliminate, astigmatism. Patients who have a different concept of their refractive outcome than the surgeon does will be unhappy. For most new refractive cataract surgeons, a goal of 85% satisfaction with postoperative vision is achievable, but the remainder of patients will need an enhancement. It is important to prepare them ahead of time for the possibility of a touchup. Patients should feel that refinement is part of the process and not a sign of failure. As surgeons sharpen their treatment nomograms, their outcomes will improve. Today, I enhance less than 2% of patients undergoing laser cataract surgery.
PERFECT THE MESSAGE
Practices must develop a cohesive value proposition and education system so that patients understand the benefits of laser cataract surgery. The first interactions patients have are with the staff, so it is important to view employees as an extension of the surgeon and provide them with the resources to learn and grow with the practice.
At my practice, we use a surgical liaison for all of our refractive cataract services. We educate patients on the value of our work and the effect astigmatic correction can have on their vision, and we develop refractive packages that are simple and straightforward.
The ideal candidate is one who understands what laser cataract surgery is and the value it can provide. Incorporating video education elements and written materials into the consultations reinforces the messaging. Additionally, our staff will follow up with patients via phone to answer questions. Actively engaging patients to partner in their care plan helps achieve a quality experience and successful outcomes.
ELIMINATE VARIABLES
I apply Six Sigma lean processes (bit.ly/SixSigmaInfo) to my astigmatic treatments to eliminate variables that negatively affect outcomes. I use the Lensar Streamline III system (Lensar) for its precision. The platform is designed specifically for managing astigmatism during cataract surgery. Imaging and biometric methods that accurately reconstruct anterior ocular dimensions determine the procedure’s safety and efficacy. The laser uses my preprogrammed nomogram with iris registration for the patient’s individualized measurements to automatically select the depth, location, and length of incisions placed for correcting astigmatism. Preoperative imaging devices that wirelessly link to my femtosecond laser facilitate the iris registration maneuver and accuracy of my planned treatments. My parameters deliver astigmatic incisions exactly on the treatment axis with 90% corneal depth through the entire chord length of the treatment at a radius of 4.3 mm from the limbal center. The best refractive cataract surgeons cannot duplicate these incisions with manual techniques.1
Although a femtosecond laser can eliminate numerous variables in corneal incisional geometry and placement, the integrity of the treatments can have variability in terms of incisional adhesiveness, not unlike LASIK flaps created with a femtosecond laser. I recommend that surgeons open all laser incisions at the time of laser cataract surgery to ensure that every treatment has the same integrity. After tabulating postoperative results for 10 or more patients, surgeons can adjust the power of the nomogram to refine future results.
DELIVER RESULTS
In my practice, refractive packages are based on delivering results for patients. I use the laser in every package, either to treat the corneal cylinder for monofocal and presbyopia-correcting IOL procedures incisionally or to mark the cornea for toric IOL placement. For astigmatic incisions, my mean postoperative refractive cylinder at 3 months is 0.17 D, with 82% of patients with less than 0.25 D of astigmatism and 95% of patients with less than 0.50 D of astigmatism (Figure).
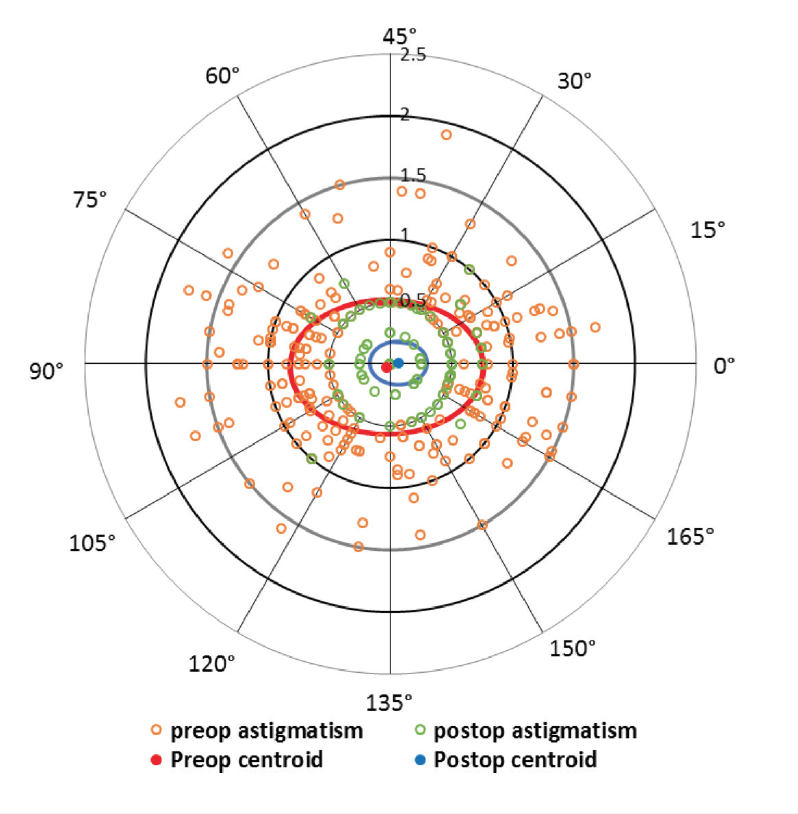
Figure. Astigmatic incision outcomes. Double-angle plots for corneal astigmatism using keratometry measurements preoperatively (blue circles) and 3 months postoperatively measured using subjective refraction (red circles). Vector analysis of astigmatism showed an improvement in J0 and J45 vectors, with a mean residual astigmatism of 0.17 D.
Toric lenses can rotate or be implanted a few degrees off axis, which necessitates a future enhancement (see the article on managing misaligned toric IOLs on p. 52). Once placed, incisions never rotate, and creating them with an iris-registered femtosecond laser means they are always on target. Lean management of my surgical processes has produced a system that is superior to my toric IOL treatments, which leave a slightly lower percentage of my patients with less than 0.50 D of residual refractive cylinder.
1. Hoffart L, Proust H, Matonti F, et al. Correction of postkeratoplasty astigmatism by femtosecond laser compared with mechanized astigmatic keratotomy. Am J Ophthalmol. 2009;147(5):779-787.