
With an ever-increasing array of IOL options, cataract consultations have become relatively involved. Patients are confronted with a tremendous amount of new information in a very short period of time, and they are asked to make important decisions about how they want to see postoperatively. During the consultation, ophthalmologists gather clinical data, formulate recommendations, and attempt to communicate several complex concepts to patients who may be apprehensive or confused. In many cases, surgeons know precious little about their patients’ daily lives, personalities, and visual desires. When one type of IOL was appropriate for almost everyone, preoperative counseling was much simpler.
AT A GLANCE
• With an ever-increasing array of IOL options, cataract consultations have become relatively involved.
• In 2004, Dr. Dell developed a questionnaire to quickly establish a common vocabulary with patients, assess how they wanted to see postoperatively, and determine if they were flexible enough to handle the optical compromises needed for success with presbyopia-correcting IOLs. He has now released an update.
• The real value of the tool is that it subtly alters patients’ expectations regarding spectacle independence and dysphotopsias.
The first major shift in thinking regarding cataract surgery occurred when achieving good distance UCVA became practical. Contributing factors included improved biometry and formulae, advances in astigmatic correction, and the rise of corneal laser refractive surgery as an enhancement tool. As presbyopia-correcting technology improves, good uncorrected distance and near vision are becoming a common goal for many patients. How do surgeons efficiently and effectively approach the preoperative consultation?
THE FIRST QUESTIONNAIRE
In 2004, I created a cataract and refractive lens exchange questionnaire to address a growing problem in my clinic. I had participated in clinical trials for early presbyopia-correcting IOLs, and upon their commercial release, I suddenly had many new options to discuss with patients. These consultations bogged down my clinic, and in some cases, lengthy discussions ended with a patient’s sudden disclosure that he or she had felt no interest in presbyopic correction in the first place. I needed a way to quickly establish a common vocabulary with patients, assess how they wanted to see postoperatively, and determine if they were flexible enough to handle the optical compromises needed for success with early presbyopia-correcting IOLs. The questionnaire was very successful in achieving these goals, and other surgeons found it helpful as well.
THE NEW VERSION
In 2016, I developed a new version of the questionnaire that my staff and I validated in the clinic for several months (Figure). The latest iteration differs from the original in several ways. First, the update offers more streamlined language and contains references to current options for accessing reading content such as e-readers and tablets.
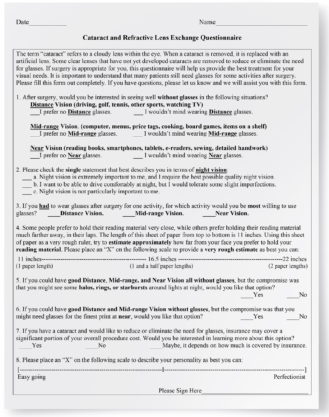
Figure. The updated Dell questionnaire.
Second, a new self-test for assessing habitual reading distance is included, owing to the variety of add powers available in multifocal IOLs today and the availability of extended-depth-of-focus and accommodating IOLs. In the self-test, patients use the vertical length of the paper of the questionnaire itself as a rough ruler to determine the distance at which they typically read. This test has been clinically validated, and it provides important feedback that may alter the IOL recommendation. If surgeons wish to use the questionnaire with a tablet or laptop computer, their patients can use a calibrated string to assess their habitual reading distance.
Another change is that the descriptions of dysphotopsias have been updated and slightly minimized to reflect current multifocal and extended-depth-of-focus IOLs.
OBSERVATIONS
Years of using the questionnaire have taught me several lessons. First, the real value of the tool is that it subtly alters patients’ expectations regarding spectacle independence and dysphotopsias. Typically, patients want total spectacle independence, but after completing the questionnaire, they understand that this outcome may not always be possible. Moreover, because the questionnaire forces them to make some difficult choices, they begin to realize that optical compromises such as dysphotopsias or loss of stereopsis may be necessary to achieve their desired spectacle independence.
A patient’s refusal to fill out the questionnaire is a red flag. The manner in which patients complete the questionnaire also yields important clues regarding their personality. Some mark up the paper with lengthy annotations, whereas others repeatedly change their answers or rewrite the questions in a fashion more to their liking. During our validation of the original version of the questionnaire, my staff and I correlated patients’ preoperative responses with their postoperative satisfaction. Of note, patients who rated their personality as exactly midway between “easygoing” and “perfectionist” tended to be the least happy postoperatively.
Nothing is a substitute for a thorough conversation with a patient, but the questionnaire allows me to enter the exam room armed with a good deal of information regarding the patient before I even meet him or her. After a dozen years of using the questionnaire, I can attest that the basic concepts it covers remain relevant and helpful. The updated questionnaire is available to download as a Microsoft Word document at crstoday.com/resources. Surgeons are free to use or modify it any way they see fit.




