

Until recently, the main surgical option for presbyopic patients wanting to depend less on reading glasses was monovision refractive correction. Corneal inlays have increased surgeons’ ability to help this population. The Kamra (AcuFocus) and Raindrop Near Vision Inlay (ReVision Optics) improve patients’ reading ability with relatively minimal impact on their distance vision. This article shares tips on optimizing your results with these technologies.
PATIENT SELECTION
Proper patient selection and preoperative counseling are the first step toward a successful result with corneal inlays. Ideal candidates for this procedure will meet your normal standards for corneal refractive surgery. Avoid patients with any ocular or systemic disease that is a contraindication for a corneal refractive procedure.
The Raindrop is indicated for patients 41 to 65 years of age who have a manifest refractive spherical equivalent of +1.00 to -0.50 D and less than 0.75 D of astigmatism. A soft multifocal contact lens trial in the patient’s nondominant eye will provide a fair simulation of the vision he or she will achieve with the inlay. The trial will thus assist you in setting a patient’s visual expectations, and it may alert you to ocular dryness concerns that can be addressed prior to surgery.
The Kamra is indicated for patients 45 to 60 years of age with a manifest refractive spherical equivalent of +0.50 to -0.75 D and less than 0.75 D of astigmatism. A refraction of -0.75 D with the inlay has been shown to provide patients with the best visual results (data on file with AcuFocus). Use of a pinhole occluder in the office will provide a fair simulation of the way this inlay will work for a patient. The AcuTarget HD (Visiometrics) is specifically designed to assist your selection of patients for the Kamra, but the device also works well for screening the ocular surface of any refractive surgery candidate. The AcuTarget HD helps to evaluate a patient’s quality of vision by quantifying light scatter through the eye and assessing the quality of the tear film. The device is also able to measure depth of focus, and it provides a guide to assist with the inlay’s placement.
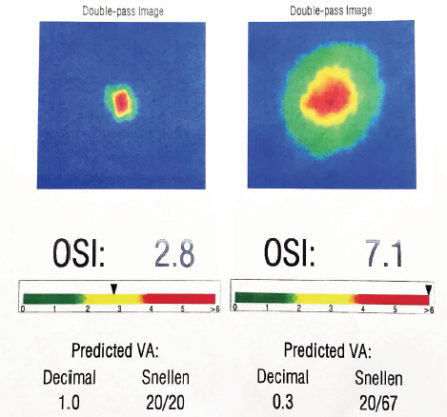
Figure. One day after receiving the Raindrop inlay, this patient presented with 20/40 distance UCVA in the operative eye, J1 at near, and an objective scatter index (OSI) of 7.1, as measured with the AcuTarget HD. He reported significant blur despite good measured acuity. One week later, he returned with the same measured acuities but an improved OSI of 2.8. The patient reported that he was now able to read easily and was very happy with his vision. The OSI measurement quantifies quality of vision based on light scatter. Specifically, postoperatively, as long as lens clarity remains stable, the device provides a useful quantitative measurement and visual picture of the effect of ocular surface dryness.
Before surgery, take the time to educate patients on reasonable visual expectations, the duration of healing, and the need for them to comply with medical treatment and follow-up. Avoid operating on patients with unrealistic postoperative expectations.
OCULAR SURFACE
Candidates for corneal inlays should be screened for ocular surface disease. Treat dry eye disease (DED), if present. The patient should have a stable, clear cornea before being considered for corneal inlay surgery. Postoperatively, the quality of the ocular surface has a direct impact on the quality of vision the patient experiences. Aggressive management of the ocular surface prior to surgery, even if significant DED symptoms or findings are absent, will both help patients understand the importance of the ocular surface and encourage their compliance with treatment after surgery.
A punctal plug can be placed in the lower puncta at the time of surgery or during the early postoperative period. Encourage patients to use artificial tears frequently. Additional treatments such as cyclosporine ophthalmic emulsion 0.05% (Restasis; Allergan) or lifitegrast ophthalmic solution 5% (Xiidra; Shire) may be necessary to maximize the health of the ocular surface. In Kamra patients, the presence of a blue ring on topography indicates tear film irregularity that will resolve with appropriate management of the ocular surface (data on file with AcuFocus; Figure).
POSTOPERATIVE MANAGEMENT
Postoperative follow-up examinations are necessary for evaluating the ocular health of patients who receive a corneal inlay. These visits are also an important opportunity for you and your staff to educate patients about and assist them with neuroadaptation to the technology. Instruct your technicians to use the reading lamp and instill an artificial tear in the patient’s eye prior to checking his or her near visual acuity. This process helps to reinforce the importance of good lighting and ocular surface management to achieve the best quality of vision. Encourage patients to decrease their use of reading glasses as much as possible to facilitate the process of neuroadaptation.
When examining the patient postoperatively, assess the flap or pocket for normal healing (no diffuse lamellar keratitis, epithelial ingrowth, etc). You can evaluate the inlay’s centration at the slit lamp by occluding the nonsurgical eye and asking the patient to focus on the slit beam. Another option for assessing the Kamra’s position is the AcuTarget HD. If an inlay is significantly decentered, you may need to reposition the device for the patient to gain maximum function.




