CASE PRESENTATION
A 65-year-old man is referred with blurred vision in his right eye. The patient underwent cataract surgery with implantation of an AcrySof IQ Restor IOL +3.0 D (Alcon) in both eyes in August 2015. He has been happy with the distance and near vision in his left eye. A residual myopic error in his right eye was subsequently treated with radial keratotomy (RK). The procedure was not successful in addressing the patient’s visual symptoms, and he presents with blurred vision in his right eye at distance and near as well as significant glare and halos.
Upon examination, the patient’s UCVA measures 20/60 at distance and near in his right eye, with a manifest refraction of -0.75 +1.25 × 127. He has a UCVA of 20/25 at distance and 20/25 at near in his left eye, with a manifest refraction of -0.25 = 20/20. Manifest refraction is +0.50 -1.25 × 37 for a BCVA of 20/25 OD. A slit-lamp examination of the right eye shows four RK incisions, with the inferior nasal radial incision extending into the visual axis (Figures 1-3). The multifocal lenses in both eyes are well centered, and both posterior capsules are intact and clear. The fundus examination is unremarkable.
How would you attempt to alleviate this patient’s blurred vision? What are your thoughts regarding the original approach of RK over a multifocal IOL to decrease residual refractive error? Is corneal incisional surgery a reasonable approach to correct residual refractive error? Would you focus on additional corneal refractive surgery or opt for lens-based surgery?
—Case prepared by William F. Wiley, MD.
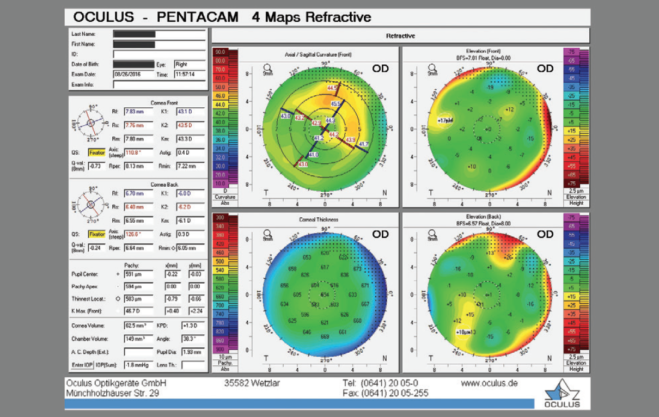
Figure 1. Imaging with the Pentacam (Oculus Surgical).
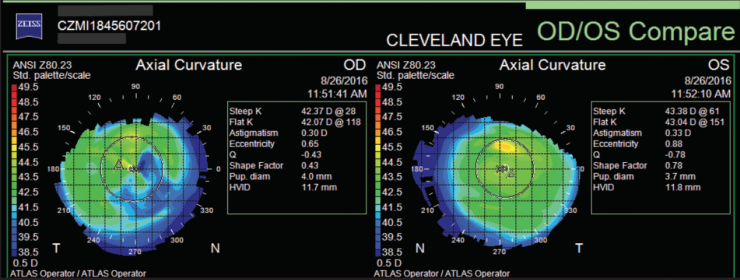
Figure 2. Topography.
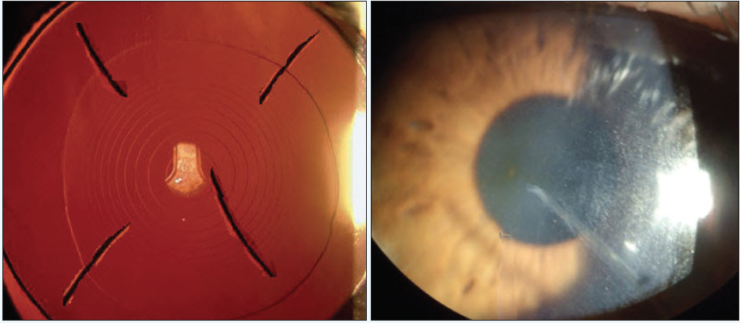
Figure 3. A slit-lamp examination shows four RK incisions (A), with the inferior scar extending into the visual axis (B).

BRYAN LEE, MD, JD
I would not perform RK over a multifocal IOL to correct residual refractive error. I find that a limbal relaxing incision works well for mild residual astigmatism if the spherical equivalent is correct, but for other errors, I would offer laser vision correction. Although surgeons without access to an excimer laser sometimes employ RK, the procedure is less accurate and less stable, and it induces more irregular astigmatism and higher-order aberrations, which significantly degrade the quality of vision with a multifocal IOL. I strongly recommend partnering with a laser refractive surgeon or performing an IOL exchange instead of RK for ametropia.
Despite a BCVA of 20/25, I am concerned about the patient’s quality of vision after RK. I would have him get glasses, and if the vision proved satisfactory, then I would offer PRK with mitomycin C. Considering the irregular astigmatism seen on topography and tomography, however, I would also offer to exchange the multifocal implant for a standard monofocal IOL as an initial strategy. The cylinder in the refraction is greater than that seen on topography, so I would look carefully for any lens tilt and obtain measurements with the iTrace (Tracey Technologies) to evaluate the internal optics.
From the very beginning, I would let this patient know that a rigid gas permeable contact lens may be necessary for the best quality of vision and would inform him that I will not be able to make the right eye match the left eye (in terms of refractive outcome, quality of vision, etc.). The central scar would be hard to address because of the incision’s depth, but fortunately, patients usually see well through this type of scar.

WILLIAM PLAUCHE, MD
Based on the slit-lamp photograph and topography, it does not appear that the patient just had RK. Apparently during the procedure, something went terribly awry, and one of the incisions was placed in the wrong location within the visual axis, ultimately creating significant irregular astigmatism. If the postoperative refraction after cataract surgery was greater than about 1.25 D of myopia, then corneal incisional surgery was less appropriate. An IOL exchange would then have been a much more reasonable approach than a four-cut RK or even LASIK in a patient with a multifocal IOL.
I think incisional surgery is a useful option for treating small residual refractive errors, even in a patient with a multifocal IOL. I frequently treat up to 1.00 D of myopia and up to 0.75 D of cylinder with mini-RK outside the visual axis. I use the mini-RK nomogram described by Richard Lindstrom, MD.1 All treatments that I do are outside the 5-mm optical zone. In my experience, treatments using 5- to 8-mm optical zones produce highly predictable outcomes without unwanted visual symptoms. One cut corrects approximately 0.50 D of myopia, and two cuts on axis treat up to 1.00 D of myopia and 0.75 D of cylinder. These incisions are only 1.5 mm in length.
If this patient’s refractive error and topography remained stable over a 3-month period, I would consider performing PRK using the Advanced CustomVue procedure (Abbott) to correct residual refractive error only if he benefited from a PreVue lens (Abbott). Otherwise, I would refer the patient for evaluation to someone who could perform topography-guided PRK. I doubt that even the best treatment will resolve all of the unwanted visual symptoms, but improvement may be possible.
Lens-based surgery is no longer an option, because it will not address the irregular astigmatism.

KEITH A. WALTER, MD
I view this case as a lesson on what not to do. Using an outdated procedure (ie, RK) to try to address an unsatisfactory outcome did some harm, but luckily, it was largely limited to induced astigmatism and a small loss of BCVA.
It is to be hoped that the scar in the visual axis fades with time. An IOL exchange will not help this patient see any better, and a penetrating keratoplasty is not indicated given such good BCVA.
When I see patients like this one in my clinic whose botched surgery I did not perform, I am honest with them about their situation. If I see a reasonable low-risk fix, I proceed. In this case, I would feel under no obligation to attempt a surgical fix. Instead, I would give the patient a pair of glasses and send him on his way. Many patients like this one fare well with a well-fit rigid gas permeable contact lens, because there is a significant amount of irregular astigmatism.
I think surgeons need to learn to tactfully say no to these disasters. There would be nothing wrong with telling this patient that, although the goal was no glasses or contact lenses, that outcome was not in the cards for him. He might not like my answer, but that is fine. I would happily recommend another qualified expert for him to see. I do not know everything, but I know I would sleep well that night.
1. Lindstrom RL. Refractive surgery and IOLs—future trends. In: Chang DF, ed. Mastering Refractive IOLs: the Art and Science. Thorofare, NJ: Slack; 2008:13-14.