CASE PRESENTATION
A 7-year-old boy sustained right-sided orbital and ocular trauma from a rock thrown by a lawnmower. The patient was initially taken to an emergency room, where he was imaged and treated for a concussion. Once home, the parents noticed that the vision in the boy’s right eye was reduced and that the eye had an unusual look with a dilated pupil.
The concerned parents brought the patient to Wills Eye Hospital’s emergency room. No afferent pupillary defect was noted on examination. Visual acuity measured 20/400 OD and 20/20 OS. The external examination found several lacerations on the brow line on the right side. A slit-lamp examination of the right eye showed mild corneal edema, a small layered hyphema, multiple iris tears, and a moderately dilated pupil. A traumatic cataract was already present. The examination of the left eye was normal. The examination of the posterior segment was normal in both eyes, although the view was limited by the cataract in the right eye.
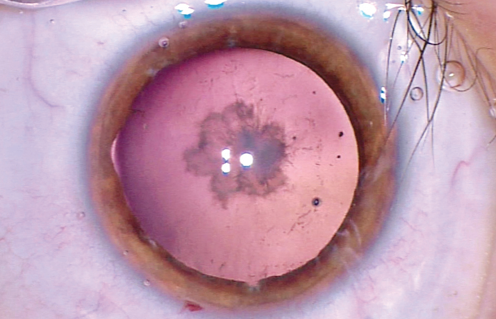
Figure 1. Traumatic cataract in a 7-year-old boy after blunt trauma to the right eye. The pupil is pharmacologically dilated, but several iris tears are visible. The patient also has anterior capsular scarring and a posterior subcapsular cataract.
The hyphema was successfully treated with cycloplegics and steroids, but the patient’s visual acuity did not return to baseline. After discontinuation of the cycloplegics, the pupil of the right eye remained dilated with minimal function. The boy was referred for a cataract evaluation and anterior segment surgery. On examination, visual acuity measured 20/200, the anterior chamber was quiet, several iris tears were evident, and the pupil measured 5 to 6 mm. The lens showed anterior capsular scarring with a moderate posterior subcapsular cataract (Figure 1). No phacodonesis was evident. The examination of the left eye was normal, and UCVA measured 20/20.
What would be the best approach to managing this patient’s anterior segment and refractive issues?
—Case prepared by Brandon D. Ayres, MD.

ZAINA AL-MOHTASEB, MD
This patient has a rosette traumatic cataract secondary to blunt trauma and anterior capsular fibrosis. Given the decreased visual acuity and the potential risk of amblyopia, I would proceed with surgical intervention with the understanding that pediatric traumatic cataracts pose unique risks when compared with those of adults. Young eyes have greater adherence between the posterior capsule and the anterior vitreous, with strong adhesions to the peripheral vitreous. Compared with adults, children are at higher risk of retinal tears, and they have a greater tendency to experience inflammation, synechiae formation, and posterior capsular opacification. Regardless of age, there is always a risk of zonular loss in patients with traumatic cataracts.
Prior to surgery, I would discuss the risks with the patient’s parents, explain that he is at increased risk of traumatic glaucoma and retinal tears, and emphasize the importance of follow-up. I would stress the necessity of establishing care with a pediatric ophthalmologist for amblyopia and refractive management.
In preparation for potential surgical complications, I would use trypan blue, and I would have capsular tension rings (CTRs) and segments in the room. I would start the capsulorhexis in an area away from the anterior capsular fibrosis and incorporate the whole area within the capsulotomy. This is typically the time I would notice if significant zonular loss were present. I would hydrodelineate the lens, which will most likely be very soft, given the patient’s age. I would use a dispersive viscosurgical device to viscodissect the remaining epinuclear material and use bimanual irrigation and aspiration to remove the cortex. If the child were unable to sit for treatment with a YAG laser, I would consider a primary posterior capsulotomy because of the high risk of posterior capsular opacification.
Given the risk of glare and halos secondary to the dilated pupil, I would perform a pupillary cerclage. After inserting the IOL, I would use a 10–0 Prolene suture on a straight STC-6 needle (Ethicon) and place a cerclage suture with the help of a 24-gauge intracath catheter to externalize the needle through four paracenteses. I would bring down the suture until the pupil reached the appropriate size, and I would make sure to perform a thorough retinal examination postoperatively.

JESSICA CIRALSKY, MD
Before proceeding with cataract surgery, I would wait until the eye was completely quiet after the initial trauma. I would make sure that the corneal edema and hyphema had fully resolved. Because the patient is 7 years old, I would not be concerned about causing amblyopia by waiting a few weeks or months.
Pediatric cataract surgery can be challenging. I would start with clear corneal incisions and would close all wounds, including paracenteses, at the end of the case with 10–0 dissolvable sutures. The anterior capsule in children is extremely elastic, which can make the creation of the capsulorhexis more difficult. I have found the addition of trypan blue aids in capsulorhexis creation by enhancing visualization and by providing capsular stiffening. I also use a heavy viscoelastic to flatten the anterior capsule. I would consider using intraocular scissors to complete the capsulorhexis if I encountered significant scarring.
Given the history of trauma, I would avoid hydrodissection. Children’s cataracts are typically soft and do not require phacoemulsification. I would remove the lens with irrigation and aspiration. I would defer a primary posterior capsulotomy if the patient is a cooperative 7-year-old who could sit for a YAG capsulotomy later on, if necessary.
I would place a one-piece IOL in the bag if the bag and zonules were intact. Typically, I would aim for an approximately +1.00 D result in a 7-year-old. Because this is a unilateral cataract, however, I would take into account the refraction in the other eye and modify the target if needed to avoid anisometropia.
Lastly, I would use an iris cerclage suture to fix the traumatic mydriatic pupil using a 10–0 Prolene suture.

KEVIN M. MILLER, MD
The first issue to be addressed is the boy’s visual acuity. Why is it limited to 20/200? Was he refracted? Would results with a pinhole test or potential acuity meter be better around the cataract? I would order macular optical coherence tomography to rule out commotio retinae and a lamellar hole. The presentation states that the patient does not have an afferent pupillary defect, so that reduces the odds of traumatic optic neuropathy.
Optical rehabilitation will necessitate cataract surgery and management of the pupillary defect. Despite the absence of phacodonesis on examination, I would implant a CTR. The device would make it easier to manage any late problems with the capsular bag that arose.
I would implant a monofocal lens and target the eye for distance vision. I would warn the patient’s parents that he will be presbyopic immediately after surgery and that he will likely become myopic in the years to come. An early laser capsulotomy will be necessary.
I would try a miotic agent such as pilocarpine to see if it constricted the pupil.
Surgical options for the pupil include suture repair and artificial iris implantation. A 10–0 Prolene purse-string pupilloplasty would be my first choice. The parents should be warned that the postoperative pupil will not be perfectly round and will not dilate. To receive a custom artificial iris device, the patient would have to enroll in an ongoing clinical trial as a compassionate-use subject. An artificial iris would have to be trephined to about 9.5 mm and placed inside the capsular bag to avoid uveal contact.

WHAT I DID: BRANDON D. AYRES, MD
After an extensive discussion and informed consent with the patient and family, cataract surgery with possible iris repair was planned and scheduled.
In eyes with prior trauma, one never knows how extensive the damage is until surgery is underway. In this boy, it was imperative to create a continuous capsulorhexis, because it would serve as the springboard for the rest of the surgery. I instilled trypan blue to enhance visualization and to change the consistency of the anterior capsule, making it behave more like an adult anterior capsule (Figure 2).
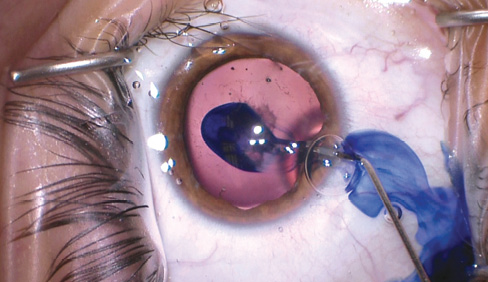
Figure 2. The surgeon stained the anterior capsule with trypan blue. Not only did the dye assist with visualization of the capsule, it also changed the “feel,” making a pediatric capsule act more like an adult’s. Even with the stain, the capsule was much more elastic than in an adult.
To tear the capsulorhexis, I used an ultrafine microrhexis forceps (MicroSurgical Technology; Figure 3) to maximize visualization and stability of the anterior chamber. The added precision helped me while tearing the capsule around the area of fibrosis.
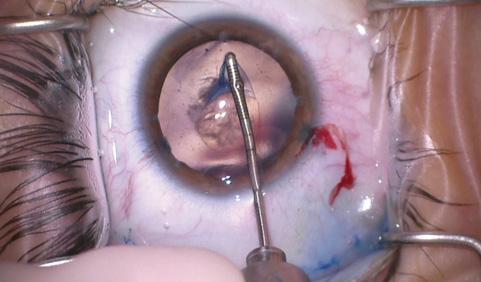
Figure 3. Dr. Ayres used a microrhexis forceps to tear the continuous curvilinear capsulorhexis. In this case, it was essential to perform the tear around the area of capsular fibrosis. The very fine jaws of this instrument provided the precise control needed in this case.
Once the capsulorhexis was complete, I removed the lenticular material with bimanual irrigation and aspiration (no phacoemulsification needed in a 7-year-old) and placed a CTR. I opted to implant a lens in the capsular bag with a target postoperative refraction of +0.75 D.
After finishing the cataract portion of the case, I instilled a miotic agent to constrict the pupil and highlight the tears in the iris sphincter. In this case, I did not want to use an iris cerclage suture, because the iris sphincter was partially functional, with interruptions from several traumatic sphincter tears. I repaired several of the tears with a sliding knot technique and left the normal iris to function. At the conclusion of the case, the pupil had a normal anatomic appearance and covered the edges of the implanted IOL (Figure 4).
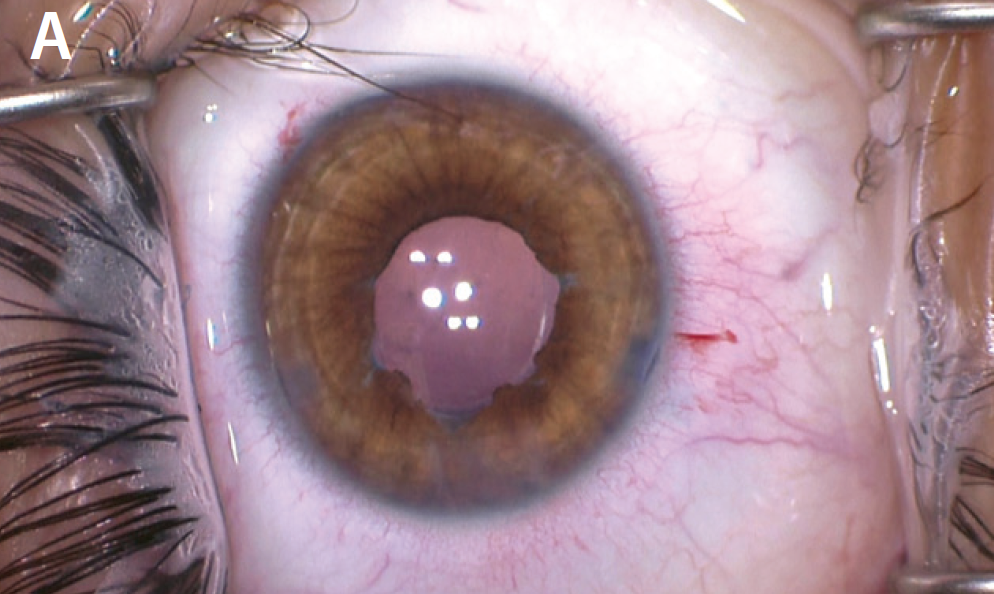
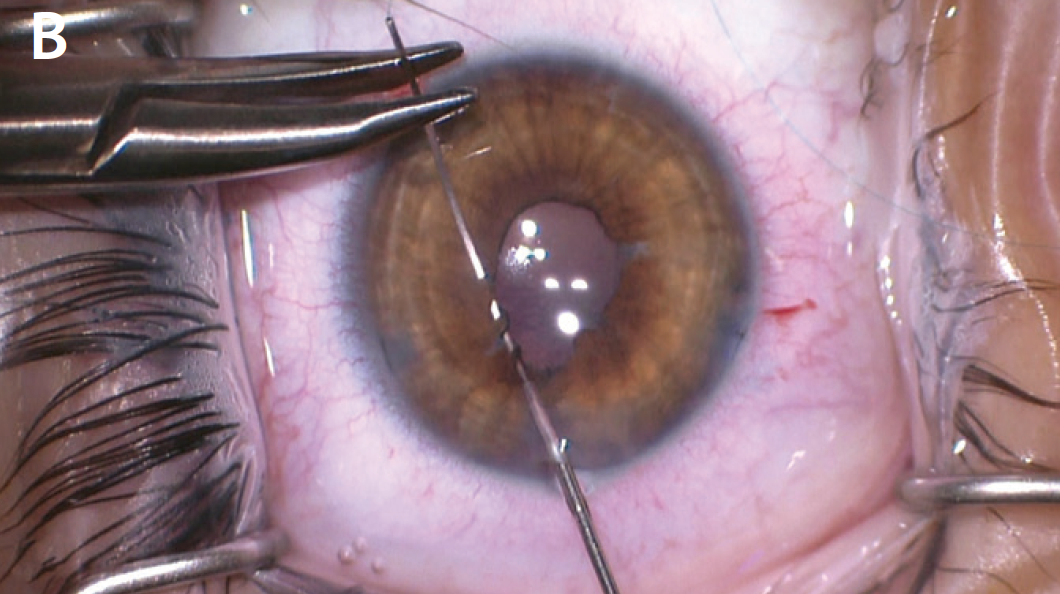
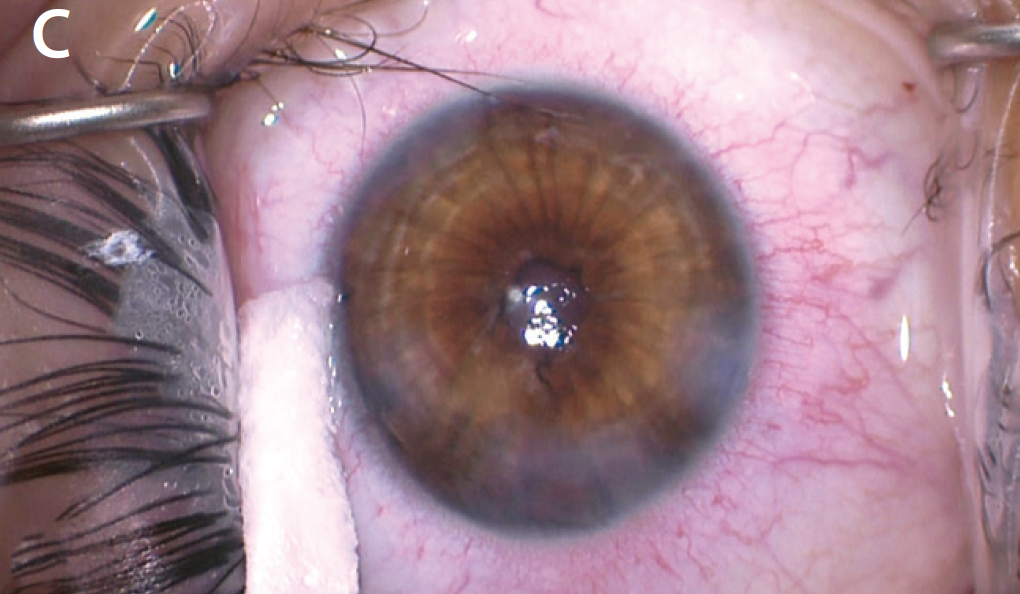
Figure 4. The iris after placement of a miotic agent, which helped to highlight the location of the sphincter tears (A). The surgeon performed several small sphincter repairs while leaving normal sphincter muscle untouched in hopes of maintaining some function postoperatively (B). The postoperative appearance of the pupil (C).
On postoperative day 1, the patient had recovered a UCVA of 20/40 with a miotic pupil and minimal inflammation. At 1 week, he had no complaints of glare, his UCVA was stable at 20/40, and it corrected to 20/25 with +0.50 D. I then referred the patient to a pediatric ophthalmologist to assist with refractive management and amblyopia prevention. My hope is that, as the patient grows, his refraction will shift toward plano or mild myopia, but only time will tell.




