
Muscle-relaxing and dermal-filling injectables can be administered in quick and simple procedures with little risk to the patient and typically minimal bruising and swelling. Ophthalmologists can readily incorporate these services into their practices; however, appropriate knowledge regarding the various products and injection sites is a requirement. This article addresses botulinum toxins and dermal fillers, highlighting the common areas for placing injections and presenting tips for safe and successful administration.
BOTULINUM TOXINS
Botulinum toxins are neurotoxic proteins. There are seven types of botulinum toxin, types A through G. Types A and B are used medically to treat muscle spasms, and they have also been widely used for cosmetic purposes. All type A botulinum toxins work via the same mechanism of action, which is by cleaving synaptosomal-associated protein 25 (SNAP-25). The cleaved SNAP-25 protein is unable to mediate fusion of vesicles with the host cell membrane, preventing the release of the neurotransmitter acetylcholine.
AT A GLANCE
- Muscle-relaxing and dermal-filling injectables can be administered in quick and simple procedures with little risk to the patient and typically minimal bruising and swelling.
- Each botulinum toxin has distinct characteristics that may influence whether and when it should be administered.
- Providers who inject dermal fillers should always have a crash cart that includes hyaluronidase nearby.
Three commonly used botulinum toxins are Botox (onabotulinumtoxin A; Allergan), Xeomin (incobotulinumtoxin A; Merz Aesthetics), and Dysport (abobotulinumtoxin A; Galderma). One of the differences among them is that the vials come in different units. Botox and Xeomin come in 50- and 100-unit vials, which is pertinent if you do not have a high-volume practice. Using a 50-unit vial may cut down on wastage. In contrast, Dysport comes in 300-unit vials, which is advantageous for providers who administer a lot of injections.
Each botulinum toxin has distinct characteristics that may influence whether and when they should be administered. Dysport contains lactose, so I avoid using it in patients with severe allergies to cow’s milk protein, as this can cause small red marks. Although the marks eventually go away, this is a cosmetic procedure, so it is obvious why I avoid Dysport in those patients.
Before it is reconstituted, Xeomin can be stored at room temperature for up to 2 years; it does not need to be refrigerated or frozen. This may be important if you travel to perform injections in other areas or countries, as Xeomin can be left in your suitcase, and you do not have to worry about putting it in the refrigerator when you get to your hotel room.
Once reconstituted, all botulinum toxins must be stored in a refrigerator. They cannot be left on the shelf for too long, and they cannot be frozen because freezing kills the neurotoxin. The average dilutions are 4 to 5 units per 0.1 mL for Botox and Xeomin and 12 to 15 units per 0.1 mL for Dysport.
AREAS OF INJECTION
There are several popular areas of injection, which are described here and shown in Figure 1.
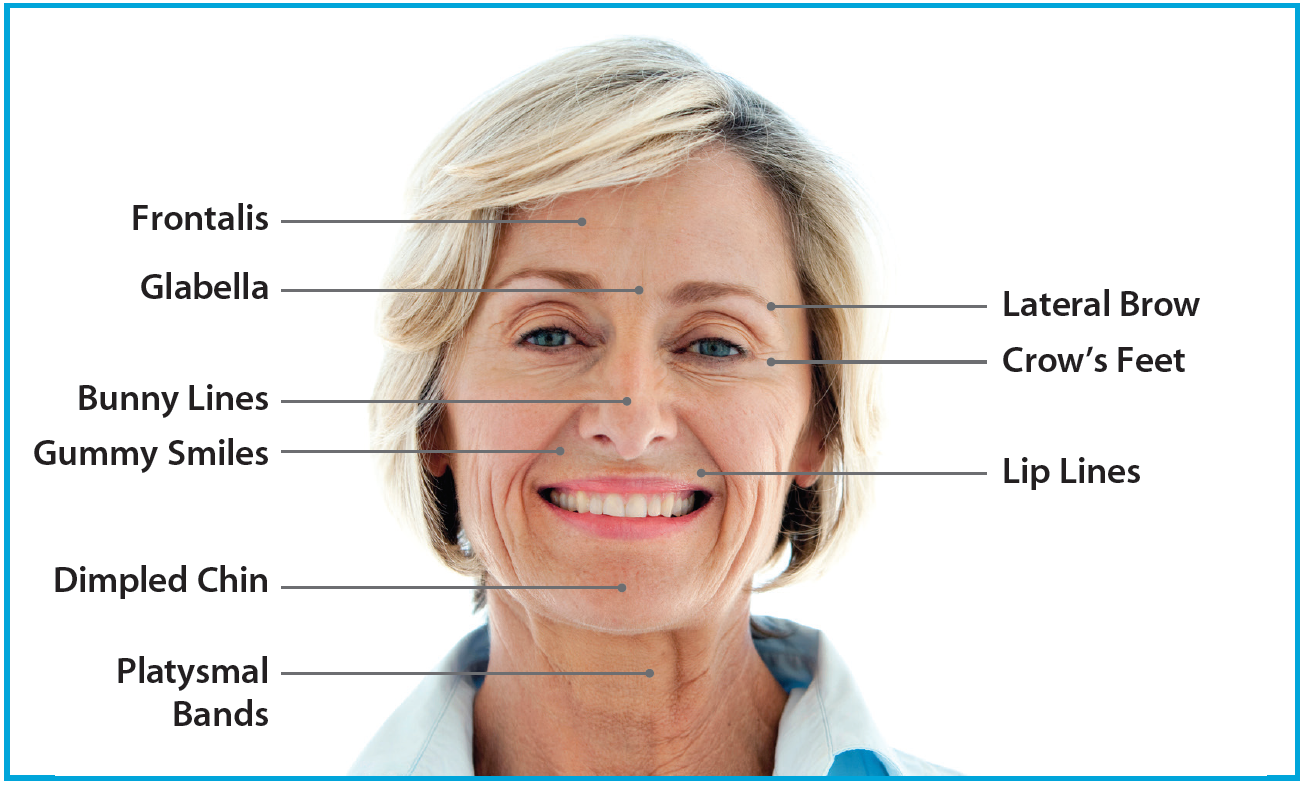
Figure. Popular areas of injection.
Glabella. The glabella is the skin between the eyebrows and above the nose. Glabellar lines, also known as the 11 lines, are created by the procerus and corrugator supercilii. Injection of a botulinum toxin can erase or soften the glabellar lines during active movement. Injections in this area also create a subtle medial brow lift because the corrugator supercilii and procerus are depressor muscles. When they are weakened, a net lift can be achieved, opening the periocular area.
Ptosis is a dreaded complication of treating the glabellar complex. It is theorized that this occurs due to the effect of the toxin diffusing through the neurovascular bundles (supraorbital and supratrochlear) toward the levator aponeurosis. Injectors can decrease the risk of this problem by using the nondominant thumb and forefinger to pinch up the muscle and protect the orbital rim. While providing protection, the nondominant hand also acts as a structure to balance the injecting hand. After the injection, I massage the toxin into the muscles and instruct the patient to remain upright for a few hours.
Frontalis. The frontalis muscle is targeted in order to soften the horizontal lines across the forehead. The frontalis is one of the most challenging muscles to inject because it is so large. It is bilobed and splits differently in different people. If you inject the frontalis and miss a certain area, you will give your patient the so-called Spock brow (for Star Trek’s Dr. Spock), as one part of the muscle is paralyzed but one part still moves.
On the other hand, if you inject too much botulinum toxin in an attempt to avoid the Spock brow, you can completely freeze the patient’s forehead and lower his or her brows. This is a particularly dissatisfying outcome for women because it hinders their ability to apply eye makeup. To avoid this, try to stay at or above the midline and use conservative doses. Additionally, I always combine frontalis with glabellar injections because the net lift from injecting the glabella counteracts the brow drop from injecting the frontalis.
There are a few situations in which I think twice about injecting the frontalis. Some people really rely on this muscle, such as those with preexisting dermatochalasis or brow ptosis. Also, Asian patients tend to have heavier eyelids and small lid creases, and they rely on that frontalis muscle. In these types of patients, smoothing out the forehead too much can prevent patients from fully opening their eyes, so caution must be taken.
Crow’s feet. Lateral canthal lines, or crow’s feet, can be rejuvenated. These injections should be superficial because the muscle is directly beneath the thin skin in this area. If you inject too deep, especially in the cheek area, zygomaticus can occur, creating a crooked smile. Keeping the injection superficial also helps avoid bruising, which is one of the telltale signs of cosmetic botulinum toxin injections.
I inject 1 to 1.5 cm lateral to the lateral canthus to avoid the lateral rectus muscle, and I am careful past the mid-pupillary line to avoid punctal ectropion. Caution should be exercised in patients with preexisting dry eye disease because their blink reflex is slightly weakened.
Lateral brow. Injection into the lateral brow area, targeting the depressive action of the lateral orbicularis oculi, can create a chemical brow lift by subtly lifting the brow about 1 to 2 mm. Combined with injections into the glabella, this can open the patient’s periocular area.
Other areas. Other facial characteristics that are common targets for botulinum toxin injections include bunny lines; the down-turning of the corners of the mouth; gummy smile; dimple chin; and vertical lip lines, also known as the barcode. Injection can also address masseter hypertrophy, a condition recognized as an enlargement of one of both masseter muscles that is common in Asian patients. Multiple injections into this area create muscle atrophy and thin the face. The platysmal bands can also be injected to create a subtle neck lift.
DERMAL FILLERS
There are many dermal fillers on the market, the most popular being hyaluronic acid. Hyaluronic acid is a natural sugar found in all living species, so it is well tolerated and unlikely to produce an allergic reaction. The beauty of hyaluronic acid is that its effects can be erased; if a complication occurs, just inject a little hyaluronidase, and the hyaluronic acid starts disappearing within 24 hours.
The commercial families of hyaluronic acid fillers include Restylane (Galderma), Juvéderm (Allergan), and Belotero (Merz Aesthetics). These differ by concentration, cross-linking, and particle size. The newest offerings from these product lines are Restylane Silk, Restylane Refyne, and Restylane Defyne ( all from Galderma) and both Juvéderm Volbella and Juvéderm Vollure (both from Allergan).
Restylane Silk and Juvéderm Volbella are indicated for use in the lips. Restylane Lyft (previously called Perlane [Galderma]), is indicated for injection into the deep dermis to the superficial subcutis for the correction of moderate to severe facial folds and wrinkles and for subcutaneous to supraperiosteal injection for cheek augmentation and the correction of age-related midface contour deficiencies.
AREAS OF INJECTION
Lines and folds. If a patient has deep lines and folds, or if I want to build the midface and cheeks, then I use a more robust hyaluronic acid such as Juvéderm Voluma, Restylane Lyft, Restylane Defyne, or Juvéderm Ultra Plus. If a patient has very fine lines and wrinkles, or if I want to fill vertical lip lines or the tear trough, I use a thinner hyaluronic acid such as Restylane, Juvéderm Ultra, Restylane Refyne, or Belotero.
Lips. Lips are a different story. If a patient wants just slight definition and not a lot of volume, then I use Juvéderm Volbella because the unique property of this product is its low concentration. If a patient wants volume, then use of a more robust product such as Restylane Silk, Juvéderm Ultra, or Belotero, is indicated.
Contents of an injectableS crash cart
If you inject with fillers, you should keep an injectables crash cart on hand. In the event of a complication—such as lumps and bumps, necrosis from an embolism in an artery, or, worst-case scenario, a central retinal artery occlusion—that crash cart is a necessity.
The crash cart should contain warm compresses that can be used to open the vascular system. The use of nitroglycerin ointment (nitro paste) is controversial, as is the use of hot compresses, because some think that dilating the vessels can push the embolism along farther.
If you are going to inject fillers, it is absolutely necessary to have a hyaluronidase in your crash cart. Vitrase (Bausch + Lomb) is ovine, and Hylenex (Halozyme Therapeutics) is human recombinant. If a vascular event occurs, flood the area with up to 450 units per cubic inch, every hour, until the embolism goes away. Necrosis is reversible, but central retinal artery occlusion is not.
CONCLUSION
Ophthalmologists can likely find success and enjoyment adding cosmetic injectables to their practices. For this reason, all of my residents receive formal training in performing injections and in proper use of all the available products. By familiarizing yourself with the types of products available and their correct areas of injection, you can ensure that injectables become a rewarding addition to your services.




