CRST asked ophthalmic surgeons and other stakeholders in the specialty what excites them about the future of ophthalmology. Robotics, genetic engineering, and microtechnology are among the areas where they foresee an abundance of action and aha moments. Their collective enthusiasm was palpable as they discussed these exhilarating developments as well as the investors eager to fund them.
Robotics
Medical technology guru and ophthalmic surgeon Richard H. Awdeh says ophthalmology is one of the first entry points to the convergence of humans and robotics, and he predicts that developments in robotics will converge with ophthalmology more as time goes on.
“The intersection of technology and humans is going to happen through the eye,” Dr. Awdeh says. Retinal prostheses, Oculus Rift (Oculus) virtual reality goggles, and MagicLeap (MagicLeap)—a virtual reality headset that relies on a photonic lightfield chip—are early examples of this, he remarks.
Retinal prosthesis developments are advancing at the Hansen Experimental Physics Laboratory at Stanford University, California. The research aims to restore sight electronically to patients blinded by degenerative retinal diseases such as retinitis pigmentosa and age-related macular degeneration. In these conditions, the photoreceptor cells slowly degenerate; electrical stimulation of the remaining retinal neurons can reintroduce information into the visual system.1 (See Watch It Now for a look at a retinal prosthesis system.)
Dr. Awdeh points out that artificial intelligence is already powerful. For example, iPhone’s Siri (Apple) can process and respond to simple questions. He notes, “When you consider the convergence of artificial intelligence and robotics, the question is, ‘How does that end up interfacing with the human?’ When is the first point that a human ends up becoming somewhat robotic or that robots become part of humans? I think that the eyes and the ears are the two intersections of technology and human bodies, so I see the opportunity for ophthalmology to play a critical role at this intersection in the next 50 years.”
Dr. Awdeh is the founder of CheckedUp (CheckedUp), a mobile health care platform focused on strengthening doctor-patient communication, as well as Cirle, the medical technology incubator responsible for the Cirle Navigation System.
INTRAOCULAR IMPLANTS
Gary Wörtz, MD, an ophthalmic surgeon and inventor of an IOL currently in development, has his finger on the pulse of the ophthalmic pipeline. He predicts that the specialty is on the precipice of the next great leap in ophthalmology. Dr. Wörtz comments, “When you look at what is going on with microtechnology, such as development in microinvasive glaucoma surgery [MIGS] and genetics- and biologic-targeted therapies as well as the understanding of disease processes and the availability of various diagnostic tools, we have an armamentarium that no generation has ever had or could even foresee. We have essentially built this war chest of understanding in one column, diagnostic technology in another column, and pharmaceutical technology in a third column. Now, we are heading into a smart device category that will interface in ophthalmology and potentially bring those three categories full circle. I think we are going to see a revolution in device technology that will really be quite astounding.” Dr. Wörtz says the IOL that he is developing through his startup, Omega Ophthalmics, is representative of that paradigm and that he is trying to play a role in creating the future.
“I see the future of ophthalmology as having intraocular implants that can do things that no one could ever imagine such as drug delivery capability, intraocular pressure sensors, continuous glucose sensors, VEGF [vascular endothelial growth factor] level meters, and potentially even sustainable long-term anti-VEGF treatment,” he says. “The years of research and development by innovators is coming to fruition. The future is so bright, and we are going to see the fruits of that labor pay off.”
LISTEN UP
Gary Wörtz, MD, invites William Trattler, MD, to describe his experience with corneal collagen cross-linking and how it is becoming the new standard of care. Listen here.
Gary Wörtz, MD, asks Ike Ahmed, MD, to share his thoughts on technologies in the pipeline for microinvasive glaucoma surgery or MIGS. Listen here.
GENETIC ENGINEERING
Ike Ahmed, MD, who has arguably done more than most to advance the trajectory of ophthalmic surgery in the past decade with his development of MIGS, says he is excited that ophthalmology is such a fast-moving field with constant innovation that can be brought forward quite easily with great success. (See Watch It Now for a look at the current state of MIGS and Listen Up for a podcast on what’s to come.)
“We are developing ways to enhance and even revive the most important sense of our body, which is our vison,” he explains. “Whether it is dealing with therapeutics in glaucoma or retina or dealing with the fascinating work being done in genetics and stem cell research, the concept that this work culminates in people being able to experience clarity and color and the beauty of our natural surroundings is pretty amazing.”
Dr. Ahmed asserts that the eye is where some of the earliest innovations in genetic engineering and stem cell research will be achieved, “because we have the tools to be able to actually see the changes in the nerve fibers right in front of our eyes.”
CAPITAL PIPELINE
Second-generation Cleveland anterior segment surgeon William Wiley plays an important role in ophthalmic innovation via his connection to the annual Caribbean Eye Meeting (his father, Robert Wiley, MD, was a founder of that meeting) as well as his own contributions to product development. Dr. William Wiley’s practice is one of the largest clinical trial investigator sites for the Light Adjustable Lens (LAL; Calhoun Vision).
According to Dr. Wiley, the capital pipeline is as vibrant as the development pipeline and shows no sign of slowing (see Follow the Money). “In medicine, there is this potential for unlimited innovation, but involvement of government and insurance companies and their influence on reimbursement [have] stifled innovation, but that is not the case with ophthalmology” he argues. “Ophthalmology is unique.”
He suggests that the out-of-pocket pay segment promotes innovation. “If you can think of something and show that it will have value to patients, it is likely that somebody will fund it,” Dr. Wiley explains. “Industry will fund it, or private equity or venture capital will fund it and push it forward knowing that novel ideas will have the potential to be reimbursed through the cash-pay segment of our specialty. This allows for limitless innovation that other specialties do not enjoy.”
GAME-CHANGING TECHNOLOGY
Vance Thompson, MD, whose résumé includes an impressive number of ophthalmic firsts, recognizes game-changing technology when he sees it. He points to three specific interventions when asked about exciting technologies in development that are poised to improve patients’ care: Oculeve (Allergan) for dry eye disease, goggles that can lower IOP on demand, and the LAL.
“As an Oculeve investigator, I have witnessed neurostimulation of the nasolacrimal reflex via the mucosa of the nasal septum come to fruition,” Dr. Thompson remarks. “I have witnessed the power of stimulating a patient’s very own natural tears and how that improves eye comfort and vision way more than artificial tears.” He believes the product could change the dry eye market.
IOP-lowering goggles are the brainchild of Dr. Thompson’s partner, John Berdahl, MD. The device can reportedly control and lower atmospheric pressure around the eye, which should lower pressure inside the eye according to the laws of physics.
“The potential ability to lower IOP with goggles to protect the optic nerve really is a game changer,” says Dr. Thompson. “Dr. Berdahl has taught me that glaucoma is a problem with pressure differentials; that, at the lamina cribrosa, there is a differential between cerebrospinal fluid pressure and IOP; and how a high IOP and a low cerebrospinal fluid pressure hurts optic nerve metabolism, axonal transport, and ultimately vision.” The goggles are designed to lessen that pressure differential at the lamina cribrosa to optimize optic nerve health.
The LAL
The LAL is another breakthrough about which Dr. Thompson is enthusiastic. “I think laser fine-tune correction has been the biggest challenge for many surgeons in premium cataract surgery,” he explains. “Patients have a specific refractive error where they will be their happiest with an implant. With this IOL, if we can do our traditional calculations and surgery to try to achieve that outcome and then, if necessary, adjust the power in the eye with a precise light treatment and lock it in when it is just right, it will revolutionize refractive cataract surgery. This is the first implant in the history of man that can be customized to the patient while in their eye.” Dr. Thompson notes that “a lot of ophthalmologists are not comfortable with delivering PRK or LASIK to adjust the final optical power of the eye after refractive cataract surgery with premium implants,” and he suggests that the LAL will make a difference. “They will be very comfortable sitting the patient up to a light delivery device that is much like sitting up and working on a patient at a YAG laser and adjusting the optical power of the lens with [ultraviolet] light,” he says. “When the patient is excited about that exact power, we can lock the implant in at that ideal power for the rest of their life.”
WATCH IT NOW
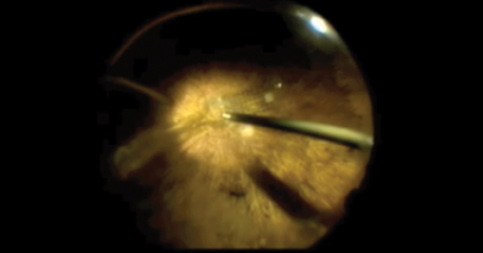
RETINAL PROSTHESIS
The Argus II Retinal Prosthesis System by Second Sight Medical Technology consists of a coil, a case that is fixed to the scleral surface, and a multielectrode array. Here, Lisa C. Olmos de Koo, MD, MBA, is shown tacking the array.
DIGITALLY ASSISTED VITRECTROMY SURGERY
Pravin Dugel, MD, joins Richard Kaiser, MD, and Jonathan Prenner, MD, for a discussion of digitally assisted vitrectomy surgery.

STATUS OF MIGS
Mark Kontos, MD, moderates a discussion with Erik Mertens, MD, and Steven Vold, MD, about the current status of microinvasive glaucoma surgery or MIGS.

TECHNOLOGY UPDATE
Avedro receives FDA approval for a second indication for its corneal collagen cross-linking platform, and Allergan files a de novo application with the FDA for the Oculeve Intranasal Tear Neurostimulator device.

TransForm
Ophthalmic innovator and entrepreneur David Muller, PhD, has a winning track record at developing and identifying interventions that transform the field—first the Summit laser for PRK and then Avedro’s corneal collagen cross-linking systems. He is at it again with TransForm (Allotex; not FDA approved), natural corneal tissue inlays and onlays that avoid the biocompatibility issue often associated with synthetic corneal inlays. Allotex is also developing a specialized desktop laser to make customizing the refractive error of the allografts easier (compared to using a clinical excimer or femtosecond laser). Dr. Muller sees the hyperopia and presbyopia markets as the initial recipients of this technology, with myopia not far behind. While Dr. Muller’s ophthalmic career has been all about the dynamic that occurs when the cornea is manipulated, when he considers the most exciting possibility in ophthalmic technology, he envisions an accommodating lens that defies past challenges. “Everything so far has been an almost,” he asserts. “The ultimate aha moment has not happened yet, but when it does, it is going to be the Holy Grail.”
1. Palanker D. Photovoltaic retinal prosthesis for restoring sight to the blind. Stanfor University Daniel Palanker’s profile page. http://web.stanford.edu/~palanker/lab/retinalpros.html. Accessed October 5, 2016.