Surgeons may not always like changes in the medical field, but many developments help them to achieve superior outcomes and better meet the demands of patients. Ophthalmologists who treat patients with glaucoma are evaluating microinvasive glaucoma surgery (MIGS) procedures that are currently available and under development. For surgeons who have hesitated to try MIGS, here are several reasons to reconsider that decision.
AT A GLANCE
• Surveys conducted at Dr. Okeke’s practice suggest that patients with concurrent glaucoma and cataract are interested in learning more about procedures that can address both conditions.
• Adding microinvasive glaucoma surgery to a practice’s offerings expands patients’ options and improves surgeons’ ability to individualize treatment.
• The safety profile of microinvasive glaucoma surgery is a key benefit of these procedures.
WHAT DO GLAUCOMA PATIENTS WANT?
Patients with this disease want to avoid vision loss and to maintain their independence, preferably without inconvenience. At present, the only way to manage glaucoma is to lower the IOP. The traditional first line of treatment is medical therapy, but long-term treatment with topical eye drops can cause side effects such as ocular surface disease and allergy with symptoms of hyperemia, foreign body sensation, burning, stinging, tearing, and a change in iris color and periorbital anatomy.1-3 Systemic side effects can include serious respiratory and cardiovascular events with the use of b-blockers.4
Poor adherence to prescribed medical therapy is a notorious problem. Patients have trouble maintaining even a once-daily drop regimen for a variety of reasons,5 including forgetfulness, cost, and difficulty with instillation as well as a poor understanding of a disease that is asymptomatic in its early stages.
My colleagues and I recently surveyed 68 glaucoma patients in our practice to ask how they felt about their drop usage. All were administering at least one IOP-lowering medication, and the majority were using one to three agents; 54% stated that their drops were expensive and/or a financial burden. Most patients (72%) were suffering from uncomfortable side effects such as burning, redness, dryness, and itching. Although 91% of those surveyed said that medical therapy represented minimal or no inconvenience, 82% were interested in learning more about procedures that could reduce or possibly eliminate their need for drops. Furthermore, 63% said they would be interested in participating in FDA clinical trials to advance glaucoma research.
We conducted another survey of 28 patients who were using topical glaucoma drops and were being evaluated for cataracts. We asked how they felt about wearing glasses and about using drops. Although 79% of patients did not mind instilling their drops and 64% did not mind wearing glasses, 86% expressed interest in undergoing a combined procedure for glaucoma and cataract that had the potential to reduce or eliminate their need for topical glaucoma medication (Figures 1 and 2).
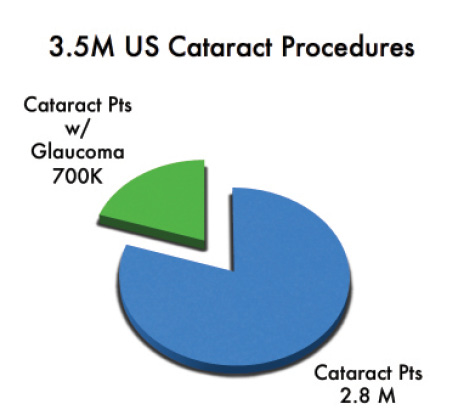
Figure 1. The MIGS treatment opportunity is significant. Abbreviation: Pts, patients. Data adapted from Centers for Medicare & Medicaid Services. 2002-2007 Medicare Analytical File. Baltimore, MD; 2007.
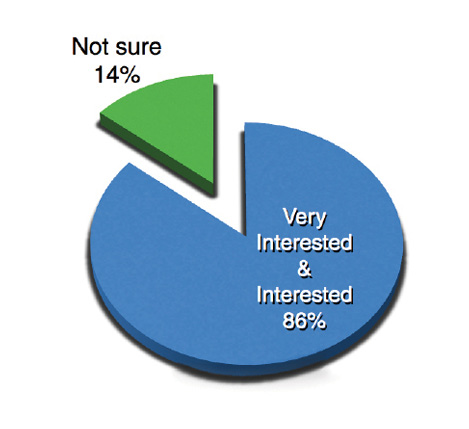
Figure 2. Our in-house survey asked 28 patients who were being evaluated for cataract surgery, “If given the option to reduce or eliminate my need for glaucoma drops with a procedure performed with cataract surgery, I would be … .”
Patients are not all the same, and glaucoma is a multifactorial optic neuropathy. I would argue that offering a variety of techniques allows ophthalmologists to best meet individual patients’ needs. Just as classes of medication work differently, it is worthwhile for surgeons to consider that MIGS procedures have multiple mechanisms of action.6
ADVANTAGES OF MIGS
For Patients
MIGS offers several benefits to appropriately selected patients. The greatest argument in favor of considering MIGS is the procedures’ safety: the risk of serious complications is far lower than with traditional glaucoma surgeries.7,8 Current MIGS procedures avoid the risks associated with a bleb. In addition, these procedures are generally performed under topical anesthesia and are completed quickly, which is a particular boon to patients who have trouble lying flat or still for a long time.
MIGS is easily combined with cataract surgery, which represents a real convenience to patients with these comorbidities. Postoperatively, healing time is similar after the combined procedure compared to cataract surgery alone.9,10 Aftercare is easier after MIGS than traditional glaucoma surgery: patients are more comfortable, owing to the lack of conjunctival sutures; they require less frequent follow-up appointments; and restrictions on their activities are lifted earlier.
Performing MIGS may delay patients’ need for more invasive glaucoma surgery, but it also keeps those options available, should they be needed in the future.
For Surgeons
Based on my experience, offering MIGS has many benefits for surgeons as well. These procedures have improved my efficiency in the OR. I can perform a combined cataract and MIGS procedure in 15 to 20 minutes, whereas traditional glaucoma surgery takes me 45 minutes to an hour to complete. Shorter cases put less strain on my back and neck muscles compared with traditional glaucoma surgery, and I can execute many MIGS procedures without fatigue. Frankly, I enjoy performing MIGS since mastering the techniques, and the safety profile of these procedures means I worry less about complications than with traditional glaucoma surgery.
Watch it Now
Constance O. Okeke, MD, MSCE, demonstrates hand positioning during a routine Trabectome procedure (NeoMedix).
Dr. Okeke shares her technique for placing an iStent Trabecular Micro-Bypass Stent (Glaukos) prior to cataract extraction.
Reimbursement also rises. For example, using physician reimbursement numbers for 2016 from the website of the Centers for Medicare & Medicaid Services, performing 27 standard cataract surgeries in 1 day ($639 × 27 = $17,253) would less than equal the physician reimbursement for 15 procedures combining Trabectome (NeoMedix) and standard cataract surgery in the same time ($839 + [$639/2] = $1,158.80 × 15 = $17,377.50). Performing 15 procedures combining the iStent Trabecular Micro-Bypass Stent (Glaukos) and cataract surgery in 1 day ($991 + [$639/2] = $1,310.50 × 15 = $19,657.50) would yield more than double the physician reimbursement of eight patchless glaucoma tube shunt surgeries performed in the same time ($1,096.69 × 8 = $8,773.52). Ambulatory surgery centers’ reimbursement for several MIGS-cataract procedures ($1,793.90 + [$976.17/2] = $2,281.99) is actually 21% more than for the implantation of a glaucoma drainage device ($1,793.90) but can take one-quarter the amount of time to perform.11
MIGS requires less chair time than traditional glaucoma surgery. Postoperative visits are the same after the combined procedure as after cataract surgery alone, which frees me up to see new patients.
With proper patient selection, MIGS can reduce IOP and/or the number of medications patients need. These results combined with effective preoperative counseling give me happy patients. I also find that offering new technologies and procedures enhances patients’ perception of my practice as cutting edge.
CONCLUSION
By increasing patients’ options with MIGS, I believe I have increased their hopefulness in the face of glaucoma, and I am better able to customize treatment to the individual. Yes, these procedures involve a learning curve, and they are not for every glaucoma patient. Proper patient selection, however, can significantly improve outcomes. For MIGS, ideal candidates have wide-open angles, ample nerve reserve, and realistic expectations regarding a reduction in IOP and/or medication burden.
1. Skalicky SE, Goldberg I, McClusky P. Ocular surface disease and quality of life in patients with glaucoma. Am J Ophthalmol. 2012;153(1):1-9.
2. Osborne SA, Montgomery DM, Morris D, et al. Alphagan allergy may increase the propensity for multiple eye-drop allergy. Eye. 2005;19:129-137.
3. Shah M, Lee G, Lefebvre DR, et al. A cross-sectional survey of the association between bilateral topical prostaglandin analogue use and ocular adnexal features. PLoS One. 2013;8(5):e61638.
4. Nelson WL, Fraunfelder FT, Sills JM, et al. Adverse respiratory and cardiovascular events attributed to timolol ophthalmic solution, 1978-1985. Am J Ophthalmol. 1986;102:606-611.
5. Okeke CO, Quigley HA, Jampel HD, et al. Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology. 2009;116(2):191-199.
6. Okeke CO. MIGS as a first-line treatment? Ophthalmology Management. February 1, 2016;20:47-49. http://bit.ly/1RRYWdj. Accessed April 12, 2016.
7. Saheb H, Ahmed II. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012;23(2):96-104.
8. Francis BA, Winarko S. Combined Trabectome and cataract surgery versus combined trabeculectomy and cataract surgery in open-angle glaucoma. Clinical & Surgical Ophthalmology. 2011;29(2/3).
9. Samuelson TW, Katz LJ, Wells JM, et al. Randomized evaluation of the trabecular micro-bypass stent with phacoemulsification in patients with glaucoma and cataract. Ophthalmology. 2011;118(3):459-467.
10. Fea AM. Phacoemulsification versus phacoemulsification with micro-bypass stent implantation in primary open-angle glaucoma: randomized double-masked clinical trial. J Cataract Refract Surg. 2010;36(3):407-412.
11. Medicare and Medicaid Programs: Hospital Outpatient Prospective Payment and Ambulatory Surgical System Payment Systems and Quality Reporting Programs; Physician-owned Hospitals: Data Sources for Expansion Exception; Physician Certification of Inpatient Hospital Services; Medicare Advantage Organizations and Part D Sponsors: CMS-Identified Overpayments Associated With Submitted Payment Data. Office of the Federal Register. http://1.usa.gov/1VxBq8g. Accessed April 25, 2016.
Constance O. Okeke, MD, MSCE
• glaucoma specialist and cataract surgeon, Virginia Eye Consultants, which has multiple locations in Virginia
• assistant professor, Eastern Virginia Medical School, Norfolk, Virginia
• migscoach@gmail.com; www.drconstanceokeke.com; Twitter @iglaucomadoc
• financial disclosure: speaker and research investigator for Glaukos; consultant to and trainer for NeoMedix; speaker for New World Medical