Case Presentation
A 62-year-old man underwent uneventful, spherical wavefront-optimized LASIK 10 years ago for the treatment of -5.00 D of myopia in both eyes. The flap was created with a microkeratome. One year postoperatively, the patient’s visual acuity measured 20/20 OU.
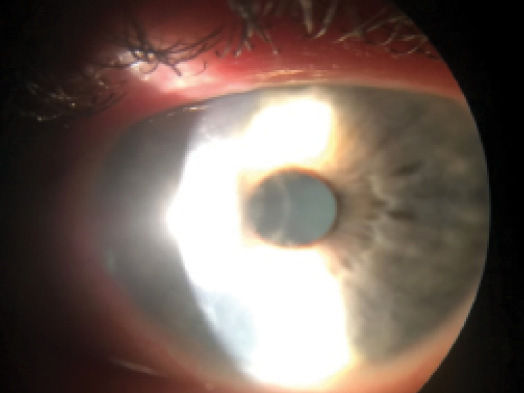
Now, the patient calls the office with a complaint of photophobia and decreased vision with pain in his right eye. Upon examination, the visual acuity of his right eye has dropped to 20/80, and he cannot tolerate light well. The cornea shows decreased sensation (Figure). The left eye is normal.
The patient reports having been placed on etanercept (Enbrel; Amgen) by his rheumatologist for psoriatic arthritis, which is systemically active at this point. The examination is otherwise uneventful.
How would you proceed with ophthalmic and systemic treatment?
—Case prepared by Karl G. Stonecipher, MD.

PREEYA K. GUPTA, MD
The patient’s symptoms are consistent with herpes simplex virus (HSV) stromal keratitis. Given the recent initiation of immunosuppressive therapy to block tumor necrosis factor (TNF), the patient is at increased risk of HSV infection and/or reactivation. The presence of a LASIK flap complicates the case in that the flap interface can be an additional site for the collection of inflammation and scar formation.
In general, I treat HSV stromal disease with topical steroids to suppress the immune reaction, and I start patients on concomitant oral antiviral therapy (such as valacyclovir, famciclovir, or acyclovir) to prevent reactivation of the virus. Post-LASIK patients with HSV are at great risk of ocular surface disease—dry eye and neurotrophic keratitis. Aggressive lubrication with preservative-free artificial tears, an artificial tear ointment, and punctal occlusion as needed is therefore important. Topical steroids should be used four to six times per day to achieve initial control of the inflammation, followed by very gradual tapering. HSV keratitis often recurs if the taper is too fast, and some patients may require long-term therapy with a low dose of topical steroids.
It would be important to address the expectations of this patient, who was used to spectacle independence. HSV keratitis is a frustrating condition for patients, and close observation is important.

JENNIFER LOH, MD
The preoperative assessment of patients considering laser vision correction (LVC) should include a discussion of their systemic conditions. For many years, patients with a history of systemic inflammatory conditions were considered to be poor candidates for LVC. A number of studies, however, have found that patients who have stable and controlled inflammatory conditions, without a recent flare, can be suitable candidates for LVC.1,2
In this case, the patient developed psoriatic arthritis many years after LVC. Although the case presentation does not mention a previous history of HSV, the presence of a disciform inflammation within the cornea is strongly suggestive of HSV stromal keratitis. Patients who are immunosuppressed may be at elevated risk of developing this corneal condition, and the presence of a LASIK flap should not influence the treatment plan.
The Herpetic Eye Disease Study (HEDS) determined that topical steroids and trifluridine work best for the treatment of HSV stromal keratitis. The study did not find that oral acyclovir hastened the resolution of an ongoing episode.3 The HEDS did determine, however, that oral acyclovir significantly reduced the risk of recurrent HSV stromal disease.4 With these findings in mind, I would start the patient on topical steroids, but I would prescribe topical ganciclovir instead of trifluridine due to a lower risk of corneal toxicity with the former. I would also have the patient begin taking oral antivirals to prevent a recurrence of the condition. In my opinion, there is no role for lifting the flap.

SHACHAR TAUBER, MD
With LASIK approaching its 20th year since FDA approval, it is not surprising that some patients who were healthy and had essentially no medical history at the time of LVC are developing systemic illnesses. Most refractive surgeons have previously healthy patients who have enjoyed many years of good vision after LASIK but are now developing an autoimmune process such as psoriatic arthritis.
Etanercept is a fusion protein of the extracellular ligand-binding portion of the human TNF receptor p75 and the Fc portion of human IgG1. This agent inhibits the action of both TNF-a and TNF-g (important proinflammatory cytokines). The drug is increasingly being used in the management of rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis, with good outcomes in both open-label and randomized controlled trials.5-8 Potentially serious but uncommon adverse effects of sepsis, reactivation of tuberculosis, worsening of congestive cardiac failure, and exacerbation of multiple sclerosis as well as reports of less serious skin reactions, lymphoma, and autoantibodies have been published. There has also been a reported case of uveitis after etanercept treatment for ankylosing spondylitis.9
There is little in the literature regarding the development of HSV keratitis after the initiation of etanercept therapy.10 The diagnosis of HSV keratitis in an immune-suppressed patient is clinical. Viral cultures and, if possible, polymerase chain reaction analysis would be of potential benefit but should not delay treatment. My suggestion would be to begin oral acyclovir 800 mg five times a day as well as aggressive treatment with a topical steroid such as difluprednate ophthalmic emulsion 0.05% (Durezol; Alcon) four times per day. Close observation to ensure that his response to this treatment was appropriate would be required. A slow taper of the topical steroid combined with conversion to a maintenance dose of acyclovir would depend on the clinical examination. It would also be necessary to guard against the rare possibility of psoriatic keratitis, which would require even more aggressive immunotherapy, but I would not stop oral antiviral prophylaxis.

KENDALL E. DONALDSON, MD, MS
This scenario is not actually uncommon but can be a diagnostic and treatment enigma. Although this case appears to be relatively straightforward, at times, the clinician may not be certain of the underlying etiology of the stromal opacity. If the patient’s diagnosis is in question or he or she is not responding appropriately to treatment, then lifting the flap with irrigation and cultures has a role in diagnosis and treatment. Atypical organisms such as Mycobacterium, Listeria monocytogenes, Acanthamoeba, or fungal keratitis may occur within the flap interface long after a patient’s LASIK surgery.11-14
Even when patients respond to a combination of antiviral and topical steroid treatment, they may have symptomatic dry eye disease associated with their neurotrophic cornea. Adjuvant therapies such as autologous serum tears, bandage contact lenses, and amniotic membranes are extremely helpful tools with which to hasten the healing of the ocular surface.
Unfortunately, many patients may not fully recover their post-LASIK visual acuity due to scarring and long-term disruptions of the ocular surface. Even a small decrease in vision may be exceedingly frustrating to this group of refractive surgery patients who are very discriminating and have high visual demands. Scleral contact lenses such as the BostonSight PROSE (prosthetic replacement of the ocular surface ecosystem) can be extremely helpful for visual rehabilitation and may provide some relief if the patient is suffering from ocular surface discomfort.
1. Cobo-Soriano R, Beltrán J, Baviera J. LASIK outcomes in patients with underlying systemic contraindications: a preliminary study. Ophthalmology. 2006;113(7):1118.e1-8.
2. Smith RJ, Maloney RK. Laser in situ keratomileusis in patients with autoimmune diseases. J Cataract Refract Surg. 2006;32(8):1292-1295.
3. Barron BA, Gee L, Hauck WW, et al. Herpetic Eye Disease Study. A controlled trial of oral acyclovir for herpes simplex stromal keratitis. Ophthalmology. 1994;101(12):1871-1882.
4. Oral acyclovir for herpes simplex virus eye disease: effect on prevention of epithelial keratitis and stromal keratitis. Herpetic Eye Disease Study Group. Arch Ophthalmol. 2000;118(8):1030-1036.
5. Safety and efficacy of etanercept in patients with psoriasis who failed to respond to other biologic treatments. US National Institutes of Health. https://clinicaltrials.gov/show/NCT00967538. Last updated July 23, 2014. Accessed January 7, 2016.
6. Observational trial with Enbrel. US National Institutes of Health. https://clinicaltrials.gov/show/NCT00488475. Last updated July 25, 2014. Accessed January 7, 2016.
7. Medication guide: Enbrel. Amgen. http://pi.amgen.com/united_states/enbrel/derm/enbrel_mg.pdf. Revised November 2013. Accessed January 7, 2016.
8. Highlights of prescribing information: Enbrel. Amgen. http://pi.amgen.com/united_states/enbrel/derm/enbrel_pi.pdf. Revised September 2013. Accessed January 7, 2016.
9. Reddy AR, Backhouse OC. Does etanercept induce uveitis? Br J Ophthalmol. 2003;87(7):925.
10. Davatchi F, Shams H, Nadji A, et al. Management of ocular manifestations of Behcet’s disease: outcome with cytotoxic drugs. APLAR Journal of Rheumatology. 2005;8:119-123.
11. Alkatan HM, Al-Dhibi HA, Edward DP, Al-Rajhi AA. Pigmented hypopyon in association with listeria monocytogenes endophthalmitis: an interesting case report following refractive surgery procedure with literature review. Middle East Afr J Ophthalmol. 2014;21(1):40-43.
12. Mittal V1, Jain R, Mittal R, Sangwan VS. Post-laser in situ keratomileusis interface fungal keratitis. Cornea. 2014;33(10):1022-1030.
13. Dolz-Marco R, Udaondo P, Gallego-Pinazo R, et al. Topical linezolid for refractory bilateral Mycobacterium chelonae post-laser-assisted in situ keratomileusis keratitis. Arch Ophthalmol. 2012;130(11):1475-1476.
14. Arnalich-Montiel F, Almendral A, Arnalich F, et al. Mixed Acanthamoeba and multidrug-resistant Achromobacter xyloxidans in late-onset keratitis after laser in situ keratomileusis. J Cataract Refract Surg. 2012;38(10):1853-1856.
Section Editor Alan N. Carlson, MD
• professor of ophthalmology and chief, corneal and refractive sur- gery, Duke University Eye Center, Durham, North Carolina
Section Editor Stephen Coleman, MD
• director of Coleman Vision, Albuquerque, New Mexico.
Section Editor Karl G. Stonecipher, MD
• clinical associate professor of ophthalmology, University of North Carolina, Chapel Hill
• director of refractive surgery, TLC in Greensboro, North Carolina
• (336) 274-2244; stonenc@aol.com
Kendall E. Donaldson, MD, MS
• associate professor of ophthalmology, cornea/refractive surgery/ external disease; medical director; and cornea fellowship codirec- tor, Bascom Palmer Eye Institute in Plantation, Florida
• (954) 465-2765; kdonaldson@med.miami.edu
• financial disclosure: consultant to and speaker for Allergan; consultant to Bio-Tissue; speaker for Physician Recommended Nutriceuticals
Preeya K. Gupta, MD
• assistant professor of ophthalmology, Duke Eye Center, Durham, North Carolina
• (919) 660-5071; preeya.gupta@duke.edu; Twitter @preeyakgupta
Jennifer Loh, MD
• comprehensive ophthalmologist in practice at South Florida Vision Associates, Fort Lauderdale, Florida
• (317) 440-7600; jenniferlohmd@gmail.com; Twitter @jenniferlohmd
Shachar Tauber, MD
• section head of ophthalmology and optometry, Mercy Clinic Eye Specialists, Springfield, Missouri
• (417) 820-2426; shachar.tauber@mercy.net
• financial interest: none acknowledged




