A 65-year-old man suffered blunt trauma in 2004 when he fell on the corner of a bookcase. The injury ruptured the globe. He underwent cataract extraction and IOL implantation in 2010.
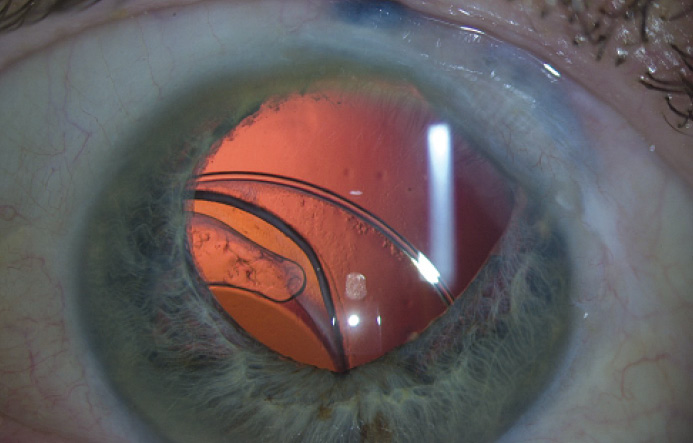
He presents with a complaint of blurred vision and severe glare in his right eye and says that he can no longer drive at night. He has a manifest refraction of -1.00 -1.00 × 95 = 20/40 OD. An examination reveals a dislocated IOL (Figure 1).
How would you proceed?
—Case prepared by
Robert K. Maloney, MD.

KENDALL E. DONALDSON, MD, MS
Given the severely dislocated single-piece acrylic IOL and capsular tension ring (CTR), the patient’s vision is surprisingly better than I would have anticipated, but I am sure it is unstable with likely diplopia. Clearly, surgical intervention is warranted before further subluxation into the vitreous occurs. The question is whether the current IOL can be salvaged or if it must be explanted and exchanged for a different lens. In the case of a single-piece acrylic lens, the answer really depends on how much capsular support is available. If there is a fibrotic capsule (possibly with a dense Soemmering ring) or a CTR (as is present here), then the IOL can be salvaged, and the fibrotic material/CTR can be used to aid fixation for scleral suturing. If no CTR or substantial capsular fibrosis is present, then I would proceed with an IOL exchange.
In this case, I would suture the CTR to the sclera using a CV-7 Gore-Tex suture (W.L. Gore & Associates; off-label use). Either two- or three-point fixation could be performed, but the latter would better avoid induced astigmatism secondary to lens tilt. Given the degree of subluxation in this case, a vitrectomy would be necessary and, ideally, would be performed through a pars plana approach to avoid anterior displacement of the vitreous. Intravitreal triamcinolone acetonide would also be useful to ensure full evacuation of the vitreous from the anterior chamber.
Alternatively, an IOL exchange could be performed, although this would be a more complex surgery, and I think simpler is always better (as described earlier). If an exchange were decided upon, I would consider two lens options: a sutured single-piece IOL with eyelets for two-point fixation (CZ70BD; Alcon) or a sutured acrylic Akreos IOL (Bausch + Lomb) with four-point fixation. With sutured IOLs, I have transitioned away from 10–O Prolene (Ethicon) to CV-7 Gore-Tex over the past 2 to 3 years for extended longevity. A three-piece IOL could be fixated in any of three ways, depending on the surgeon’s preferred technique: iris fixation, glued IOL through scleral tunnels, or sutured IOL with scleral flaps (10–O Prolene) or Gore-Tex fixation (rotated sutures). Of course, there is always the standard anterior chamber IOL; these lenses are popular in clinical practice (although unconventional at meetings), and older patients with larger anterior chamber depths do extremely well with them.1

JAMES A. KATZ, MD
The patient appears to have a dislocated IOL and CTR as well as an irregular pupil with loss of iris tissue. He would likely benefit from transscleral fixation of the IOL and repair of the iris.
Given the previous trauma and surgical repair, I have three concerns going into this case. First is the condition of the sclera. If the tissue appears too thin over the site of suture placement, I would avoid Hoffman pockets or scleral flaps. My second concern regards the condition of the conjunctiva. It may be scarred down to the sclera and difficult to reposition adequately at the end of the surgery. Finally, I would have a plan to repair the pupil without access to artificial iris implants or the ability to place modified CTRs with multiple occluder paddles in the capsular bag.
I would prefer not to open the eye for an exchange if the IOL is not damaged. I would create a conjunctival peritomy and then a partial-thickness scleral groove about 1.5 to 2 mm posterior to the limbus. If the sclera appeared too thin, I would forego the groove and later place a scleral patch graft to cover the exposed suture. I would pass a 25-gauge needle ab externo under the iris and through the posterior capsule. Through a paracentesis 180º away, I would use a double-armed CV-8 Gore-Tex suture on a flattened needle to dock to the 25-gauge needle out through the scleral groove. The second pass would be made about 2 mm away and passed on top of the IOL complex. The other end of the Gore-Tex suture would be fed through the same paracentesis and docked to the 25-gauge needle out through the scleral groove to create a continuous loop around the haptic. I would place a knot to allow centration of the IOL. This same procedure might need to be performed 180º away. The knot would then be rotated into the eye and the conjunctiva replaced into position. If the conjunctiva could not be reapposed, I would place amniotic membrane over the exposed sclera.
After instilling acetylcholine to constrict the pupil, I would attempt to repair the iris using 10–O Prolene on a CIF-4 needle. The needle would be placed through the peripheral cornea, through the anterior margin of the iris, and out the posterior margin, approximating the tissue the same distance to the limbus on both sides. I would bring the suture ends out of a paracentesis and tie them using a Siepser knot. This process could be repeated in the midperiphery of the iris to reduce the resultant peripheral iridectomy.
Surgical planning using these techniques would likely improve the patient’s vision and decrease glare.

MICHAEL E. SNYDER, MD
This subluxated IOL-capsular bag complex is inducing symptoms for the patient. Moreover, the situation is unstable; with time or trivial trauma, the complex could frankly subluxate into the posterior segment. Given no systemic contraindications to surgery and the patient’s willingness to proceed, I would recommend repositioning this complex.
First, if present, any offending vitreous gel would need to be cleared from the area. I would perform a conjunctival peritomy superonasally and create two 23-gauge openings in the scleral wall at the level of the sulcus about 3 to 4 mm apart. With the anterior chamber filled with an ophthalmic viscosurgical device and an anterior chamber maintainer placed inferonasally, I would pass a 25-gauge microforceps through the scleral wall opening and under the edge of the CTR at roughly the 1:30 meridian, while I passed a second microforceps, preloaded with the blunt end of a CV-8 Gore-Tex suture, through an inferotemporal paracentesis transcamerally to the same site. I would rub the tips together to pierce the fused peripheral anterior and posterior capsules until one tip passed through the plane.
Next, the suture end would be handed off to the scleral wall forceps (Figure 2) and pulled out of the eye. I would then place the forceps through the other scleral wall opening and pass the other end of the Gore-Tex suture to it, this time over the capsular complex, effectively looping the CTR. The suture would be gently tied externally with just enough tension to maximize the centration of the IOL. Subsequently, I would tuck the knot internal to the eye wall and close the conjunctiva and Tenon fascia with an absorbable suture. After removing the ophthalmic viscosurgical device, I would administer intraocular carbachol for maximal IOP control postoperatively.
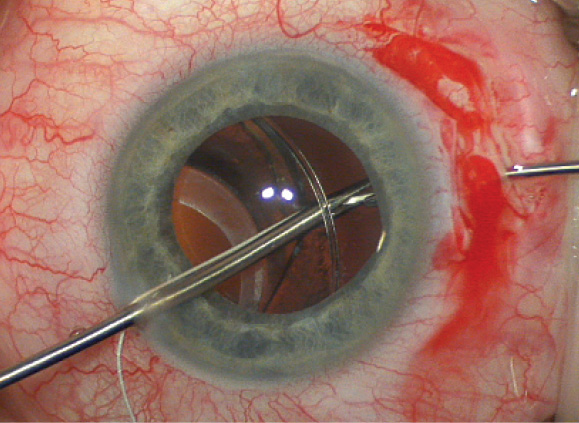
Figure 2. The forceps through the paracentesis has pierced the fused capsules, just inside the CTR. The Gore-Tex suture in the jaws of this forceps is being handed off to the microforceps through the scleral wall.
It is unlikely that this iris defect can be closed with sutures, although sometimes, the iris can be more elastic than expected. A customized iris prosthesis would be an excellent option, but if used in the United States, it would need to be within the confines of the FDA investigational device exemption study at this time.
The hint of scleral thinning in Figure 1 might benefit from a patch graft, but not enough information is provided to definitively comment on this issue.
Although a limbal relaxing incision could likely reduce the astigmatism, the spherical outcome would not be clear until the eye healed, because the current refraction may be unreliable, given the IOL’s position. n
1. Donaldson KE, Gorscak JJ, et al. Anterior chamber and sutured posterior chamber intraocular lenses in eyes with poor capsular support. J Cataract Refract Surg. 2005;31(5):903-909.
Section Editor Alan N. Carlson, MD
• professor of ophthalmology and chief, corneal and refractive surgery, Duke University Eye Center, Durham, North Carolina
Section Editor Stephen Coleman, MD
• director of Coleman Vision, Albuquerque, New Mexico
• (505) 821-8880; stephen@colemanvision.com
Section Editor Karl G. Stonecipher, MD
• director of refractive surgery, TLC in Greensboro, North Carolina
Section Editor William F. Wiley, MD
• private practice at Cleveland Eye Clinic, Cleveland, Ohio
Kendall E. Donaldson, MD, MS
• associate professor of ophthalmology, cornea/refractive surgery/ external disease; medical director; and cornea fellowship codirector, Bascom Palmer Eye Institute, Plantation, Florida
• (954) 465-2765; kdonaldson@med.miami.edu
• financial disclosure: consultant to Abbott Medical Optics and Alcon
James A. Katz, MD
• director, Golf Laser Vision, The Midwest Center for Sight, Des Plaines, Illinois
• (847) 824-3127; jkatz@tmcfs.com
• financial interest: none acknowledged
Michael E. Snyder, MD
• member, Board of Directors, Cincinnati Eye Institute
• volunteer faculty, University of Cincinnati
• (513) 984-5133; msnyder@cincinnatieye.com
• financial disclosure: consultant to HumanOptics, the manufacturer of the custom iris device


