A 64-year-old woman is referred to you by her ophthalmologist for a cataract evaluation. The patient underwent implantation of Intacs intrastromal corneal ring segments (Addition Technology) in 1999 for the treatment of myopia. She reports being happy with her vision after surgery until 2 years ago, when it gradually started to worsen. She no longer drives at night due to decreased vision.
The patient’s manifest refraction is -2.00 +0.75 × 013 = 20/30- OD and -5.25 +1.00 × 140 = 20/50 OS. Glare testing reveals decreased visual acuity of 20/80 OD and 20/200 OS.
Testing with the Pentacam (Oculus Surgical) shows mild astigmatism in her right eye with corneal flattening but no evidence of keratoconus: 39.0/40.2 × 15 OD and 39.6/39.9 × 100 OS.
A slit-lamp examination reveals well-positioned intrastromal corneal ring segments oriented at 90º in both corneas (Figure). The patient has 2+ nuclear sclerosis with an early posterior subcapsular cataract in her right eye and 2+ to 3+ nuclear sclerosis with a 1+ to 2+ posterior subcapsular cataract in her left eye. The remainder of the examination is normal, and a dilated funduscopic examination is normal.
How would you approach cataract surgery for this patient? Would you consider removing the ring segments before the procedure? If so, how long would you wait to perform surgery after explantation. Which IOL power calculations would you use, and which IOLs would you consider?
—Case prepared by Audrey R. Talley Rostov, MD.
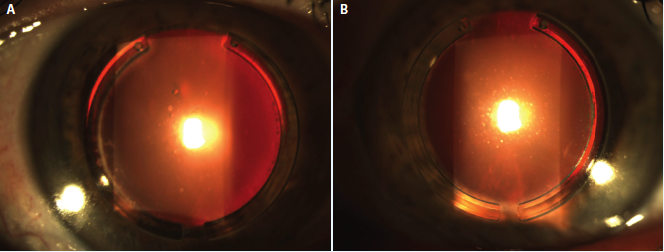
Figure. Well-positioned intrastromal corneal ring segments oriented at 90º in the patient’s right (A) and left (B) eyes, which both have developed cataracts.

ARTHUR B. CUMMINGS, MB ChB, FCS(SA), MMed(Ophth), FRCS(Edin)
This is the first time that I have been challenged with this particular set of circumstances. I see three clear options.
The intrastromal corneal ring segments have been in the eyes for 17 years now and are not causing any problems at all. One could simply proceed with cataract surgery after warning the patient that there is a greater-than-usual chance of not achieving the refractive target because of the altered cornea. The advantage of this strategy is the potential for only one procedure (the cataract surgery). The disadvantage is that the segments remain in the eyes and may have to be removed in the future.
A second option is to remove the devices now and to perform serial topographies at 6 weeks and 3 months. If topography is stable at 3 months, standard cataract surgery could proceed using current IOL formulae. In the interim, the patient will probably require glasses to correct the increased myopia after the segments’ removal. If the topography were not stable, I would repeat the measurements every 6 weeks until they stabilized. The advantages of this strategy are that removing the implants will prevent their potentially causing problems in the future and that IOL power selection will likely be more accurate. The disadvantage is that this approach commits the patient to two procedures (ring removal and cataract surgery).
A third option is to combine device removal and cataract surgery. The patient would require a clear warning that biometry will be compromised and that an enhancement procedure may be required postoperatively. The advantages of this strategy are that only one procedure may be needed and that explanting the segments will prevent their potentially causing problems in the future. The disadvantage is that IOL power calculations will be more challenging than usual, so this approach carries the greatest possibility of requiring an enhancement. I would do a calculation with current keratometry readings (Ks; flatter than before). Then, I would do one using pre-ring segment Ks (previously steeper) and deduct 120% of this keratometric change from the IOL power to be used. For example, current biometry suggests using a 20.00 D IOL, and the previous Ks used in a current calculation suggest a 17.00 D IOL; this is a 3.00 D shift. I would subtract 120% of 3.00 D from the current IOL power (ie, 3.60 D subtracted from 20.00 D) and thus choose a 16.50 D IOL.

ERIC D. DONNENFELD, MD
Intacs were originally approved for the correction of myopia but have subsequently become an important treatment for keratoconus as a means of flattening the steep axis of cylinder. In this case, the devices were successfully employed for the treatment of myopia. The decision of whether to remove or maintain the segments is an informed consent issue, because in my experience, patients do very well with cataract surgery while the implants are in place. The patient should be made aware that some individuals later (even 20 years later) develop neovascularization, extrusion, or lipid deposition in the channels that require the segments’ removal, which will change the refractive success of the cataract procedure. In addition, the devices usually create a mildly irregular cornea, which can be assessed on topography, and their removal may result in an improved quality of vision after cataract surgery.
If the decision were made to remove the Intacs, I would wait 3 months after their explantation, until two topography measurements taken 1 month apart were stable, before proceeding with conventional cataract surgery using the IOL I would select for a normal case. If the decision were made to maintain the ring segments, the central cornea would be flattened relative to the posterior cornea, and using conventional IOL formulae would likely leave the patient hyperopic. I would therefore use the American Society for Cataract and Refractive Surgery’s calculator for myopic LASIK and rely on the Barrett formula for selecting an IOL. Ideally, I would employ intraoperative aberrometry to determine IOL power and would select a lens with zero aberrations.

PAUL J. DOUGHERTY, MD
This patient’s induced myopia and decreased BCVA are obviously due to the nuclear sclerotic and posterior subcapsular cataracts. I would approach this case by recommending the removal of the Intacs bilaterally and waiting 6 months to allow the cornea to revert to its natural shape. I would document corneal stability with corneal tomography and topography 1, 3, and 6 months after the segments’ removal. Explanting the devices would obviate the need for further refractive surgery, whereas the future development of a melt or vascular ingrowth around the Intacs would require their removal and cause a loss of corneal flattening. Other advantages of removing the implants are that it will allow for better visualization during surgery and eliminate the risk of blocking laser energy into the eye if the patient undergoes laser cataract surgery.
After explanting the segments and allowing the cornea to regain its natural shape, I would employ my usual IOL calculation formulae dependent on axial length (Holladay II for normal eyes, SRK-T for long eyes, or Hoffer-Q for short eyes). In addition, I would have no problem offering the patient any of my usual IOLs according to her visual needs. If she wished to decrease her dependence on reading glasses and failed a monovision trial, I would offer to implant bilateral multifocal IOLs.

BRADLEY D. FOURAKER, MD
The patient presents with well-positioned intrastromal corneal ring segments in each eye and progressive nuclear sclerotic and posterior subcapsular cataracts, with the left eye more affected than the right. Pentacam readings suggest that the majority of the astigmatism in the right eye is secondary to the corneal curvature, whereas in the left eye, the majority of the astigmatism is lenticular.
The patient is not having any complications with the devices, so there is no reason to remove them prior to cataract surgery. Because the inner diameter of the segments is typically 6.8 mm and the outer diameter is 7.6 mm, the ophthalmologist can use his or her typical approach to cataract surgery. A temporal approach would be ideal in that the temporal corneal limbus should be several millimeters from the implants. Given the large interior ring-to-ring measurement, there is no need to adjust the power calculations.
Considering the 1.00 D of corneal astigmatism, a toric IOL would be appropriate for the right eye, whereas a spherical lens would be appropriate for the left eye. Certainly, multifocal lenses could be considered, but an astigmatic keratotomy would be minimally effective without removing the ring segments.

WHAT I DID: AUDREY R. TALLEY ROSTOV, MD
Because the patient was happy with her post-Intacs vision for 14 years until she experienced an increase in myopia from cataract formation, I decided to leave the segments in position and to proceed with cataract surgery. I have a large keratoconus practice and a number of patients who have previously had the devices placed for keratoconus on whom I have successfully performed subsequent cataract surgery.
I explained to the patient that, because of the segments and the resultant difficulty of obtaining accurate IOL power calculations, she might require glasses for some activities other than midrange and reading vision postoperatively. I added that the goal would be to obtain the best distance UCVA possible. I did not offer her the option of a multifocal IOL, because a multifocal cornea does not work well with this type of lens.
I chose to perform laser cataract surgery on her left eye with a 4.9-mm capsulotomy and phacofragmentation pattern commensurate with the density of the cataract. I do not routinely create my cataract incisions with the femtosecond laser, because I am a bimanual cataract surgeon, so I did not use the laser for the cataract incisions in this case.
Bimanual cataract surgery proceeded without complication. I attempted unsuccessfully to obtain intraoperative aberrometry readings and ultimately chose a one-piece hydrophobic acrylic IOL, the power calculated with an average of LASIK modification to the Haigis L and Shammas formulae, which was 2.00 D greater than the calculation with SRK-T and Holladay formulae. As in post-LASIK eyes, I was careful to calculate for more myopia, because the flattening effect of the Intacs can result in a hyperopic postoperative surprise if not taken into consideration.
Postoperatively, the patient is doing well, with 20/25 UCVA and a residual refraction of -0.50 +0.50 × 105 OS. She is deciding whether or not she wants to retain some myopia for a monovision approach before we schedule her right eye for cataract surgery.
Section Editor Lisa Brothers Arbisser, MD
• emeritus position at Eye Surgeons Associates, the Iowa and Illinois Quad Cities
• adjunct associate professor, John A. Moran Eye Center, University of Utah, Salt Lake City
Section Editor Brandon D. Ayres, MD
• surgeon in the Cornea Service, Wills Eye Hospital, Philadelphia
Section Editor Audrey R. Talley Rostov, MD
• private practice with Northwest Eye Surgeons, Seattle
• SightLife global partner
• (206) 528-6000; atalleyrostov@nweyes.com
• financial interest: none acknowledged
Arthur B. Cummings, MB ChB, FCS(SA), MMed(Ophth), FRCS(Edin)
• consultant ophthalmologist, Wellington Eye Clinic and Beacon Hospital, Dublin, Ireland
• abc@wellingtoneyeclinic.com; Twitter @cummingsab
• financial disclosure: consultant to Alcon and WaveLight Laser Technologie
Eric D. Donnenfeld, MD
• professor of ophthalmology at NYU, New York
• trustee of Dartmouth Medical School, Hanover, New Hampshire
• (516) 766-2519; ericdonnenfeld@gmail.com
• financial interest: none acknowledged
Paul J. Dougherty, MD
• medical director, Dougherty Laser Vision, Westlake Village, California
• assistant clinical instructor of ophthalmology, Jules Stein Eye Institute, David Geffen School of Medicine, University of California, Los Angeles
• (805) 987-5300; info@doughertylaservision.com
• financial interest: none acknowledged
Bradley D. Fouraker, MD
• in practice at the Brandon Cataract Center and Eye Clinic in Brandon, Florida
• (813) 681-1122; bfouraker@verizon.net
• financial disclosure: member of OMIC board; consultant to Alcon and Oasis Medical


