Monovision creates artificial anisometropia in order to correct presbyopia. Westsmith first proposed this technique in 1958 as a method of prescribing optical aids for presbyopic contact lens wearers.1 Monovision continues to be effectively used to manage presbyopia, with studies reporting a mean success rate of 73% using contact lenses2 and 86% to 96% after refractive surgery.3-5
Monovision in pseudophakic patients was first described in 1984.6 Owing to advances in surgical technique and IOL technology, patients pursuing cataract or refractive lens exchange surgery are increasingly demanding about their postoperative visual function and spectacle independence. Overall, patients report an 80% or higher rate of satisfaction with pseudophakic monovision.7-10 Success with this approach can be achieved with monofocal, toric, or accommodating IOLs, and it has become a vital skill for today’s ophthalmic surgeons.
PREVALENCE
Monovision correction during cataract surgery is popular among ophthalmologists. In a 2003 survey of American Society of Cataract and Refractive Surgery (ASCRS) members, 86% of US surgeons preferred monovision or modified monovision, whereas only 13% preferred multifocal IOLs.11 Even as IOL technology improved, a 2014 survey of physician attendees at the ASCRS annual meeting found that monovision correction during cataract surgery was used three times more commonly than all presbyopia-correcting IOLs (22.3% vs 7.2%). Cost to the patient, concern over nighttime quality of vision, and concern about inadequate unaided near and intermediate vision were cited as the most common barriers to converting patients to presbyopia-correcting IOLs.12
Achieving success with pseudophakic monovision requires careful preoperative planning, knowledge of the technique’s limitations, sufficient patient counseling, and excellent surgical technique.
PREOPERATIVE ASSESSMENT
In order to assess a patient’s goals, lifestyle needs, preference for glasses after surgery, and financial considerations, I use a questionnaire designed by Steven J. Dell, MD (Figure). Ideal candidates for pseudophakic monovision correction not only have a strong desire to be less dependent on glasses, but they also understand the strategy’s limitations.
A deciding factor between a presbyopia-correcting IOL and pseudophakic monovision is the patient’s level of motivation for achieving spectacle independence. The bilateral implantation of multifocal IOLs achieves higher rates of spectacle independence than does pseudophakic monovision: 78% and 81% with the AcrySof IQ Restor models SN6AD1 and SN6AD3 (Alcon), respectively, and 85% with the Tecnis ZM900 (Abbott Medical Optics).13,14 In comparison, the rate of spectacle independence after cataract surgery varies from 26% with 1.00 to 1.16 D of monovision to 81% with 2.27 D of monovision.8,9,15 Historically, patients with pseudophakic monovision have reported difficulty reading fine print and driving in dim light or hazardous conditions, but having backup glasses for these situations typically resolves the problem. Any patient considering pseudophakic monovision should have realistic expectations regarding his or her need for glasses based on the planned amount of anisometropia.
Of note, multifocal IOLs reduce contrast sensitivity and increase the prevalence of dysphotopsia, particularly glare and halos, compared with monofocal IOLs.14,16 In a direct comparison to patients with approximately 1.25 D of pseudophakic monovision, individuals who underwent bilateral multifocal IOL implantation had an increased rate of dysphotopsias and IOL exchange surgery.15
Deciding between pseudophakic monovision and multifocal IOL implantation to address presbyopia also requires a financial discussion with patients and counseling on the shortcomings of each option.
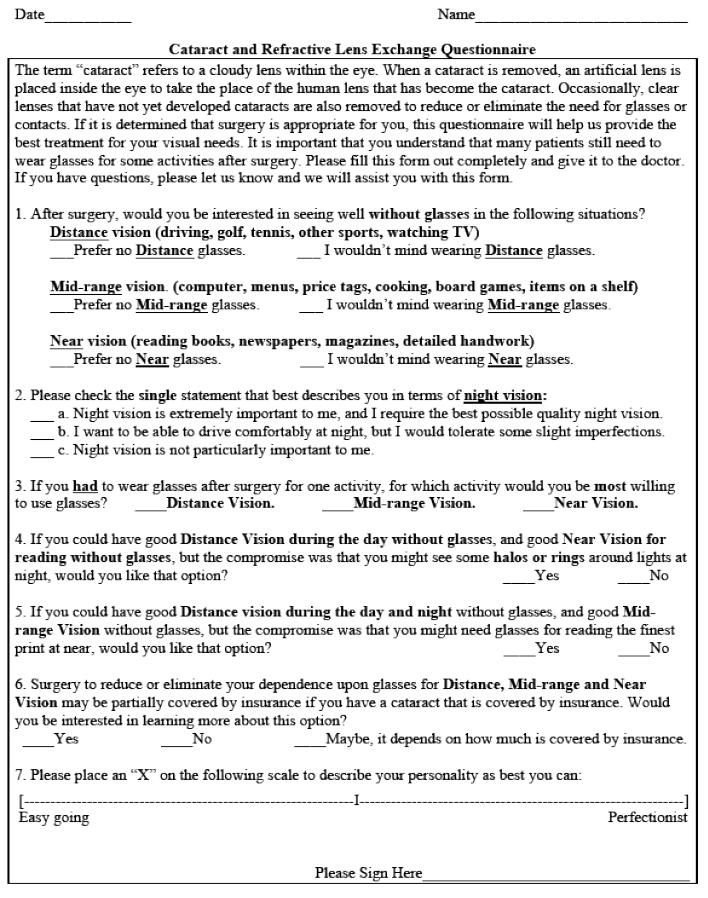
Figure. The Dell Index.
FACTORS INFLUENCING SUCCESS WITH PSEUDOPHAKIC MONOVISION
How Much Anisometropia?
In conventional monovision, surgeons historically aimed for 2.00 to 2.50 D of anisometropia, but in a 2003 survey, 46% of surgeons preferred a modified monovision approach, which targets a refraction of -0.50 to -1.00 D in the nondominant eye.11,17 Modified monovision provides patients with excellent binocular vision at far and intermediate distances, but their near vision is limited compared to after conventional monovision.18 Modified monovision is likely gaining popularity, because intermediate vision tasks such as using a mobile phone, tablet, and computer are becoming increasingly important.
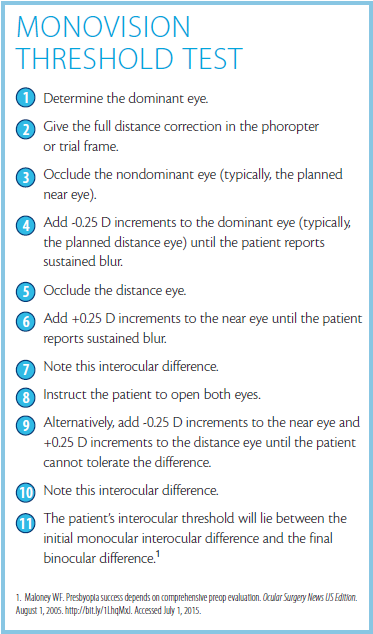
Stereopsis and contrast sensitivity are reduced in proportion to the amount of anisometropia.18 A monovision threshold test can help surgeons to determine what degree of anisometropia a given patient can tolerate (see Monovision Threshold Test).19
Of note, monofocal IOLs have pseudoaccommodative properties because of the depth of focus, miosis upon convergence, lid squeezing, the implants’ spherical aberration, corneal multimodality, or postoperative refraction.20 This additional 1.00 D of accommodative effect usually means that the myopic defocus in pseudophakic monovision can be limited to 1.50 to 1.75 D yet still provide a greater range of vision.21
Although recommended for patients undergoing keratorefractive surgery, a contact lens trial with monovision may be of limited utility in cataract surgery patients owing to their poor BCVA.22 I have found it beneficial to place a +1.25 D trial lens in front of the planned near eye when I am explaining the expected outcome to one of these patients.
The Role of Ocular Dominance
Because patients with strong ocular dominance will not be able to suppress blur, lower levels of anisometropia should be considered for these individuals.19
Oftentimes, the dominant eye is corrected for distance based on the assumption that the nondominant eye will more easily suppress blur. There are reports of success with crossed monovision, however, so perhaps the magnitude of ocular dominance is more significant in determining patients’ satisfaction.4,7
Other Considerations
Success with pseudophakic monovision demands an emmetropic result in the patient’s distance eye. For that reason, surgeons must correct astigmatism via astigmatic keratotomy, limbal relaxing incisions, laser vision correction, and/or toric IOLs.
A patient’s age matters. In one study of pseudophakic monovision, the highest percentage of satisfied patients were 70 years of age or older.8
Pseudophakic monovision may compromise vision in low light such as when patients are driving at night. The procedure can also decrease depth perception. It is therefore important for surgeons to consider the patient’s occupation and hobbies preoperatively.
Further studies of pupillary size are needed. Generally speaking, surgeons should be conservative about the amount of myopic defocus in patients with large scotopic pupils.19
Monovision should be avoided in patients at risk of developing postoperative diplopia such as those with a history of strabismus surgery, phoria, or intermittent tropias.22
When a patient is not a candidate for a multifocal IOL but is highly motivated to achieve spectacle independence, surgeons can consider using a myopic defocus with an accommodating IOL such as the Crystalens or Trulign (Bausch + Lomb). Because of the limited accommodating ability of these IOLs, pseudophakic monovision is necessary to achieve high rates of spectacle independence.23 In my experience, when implanting accommodating lenses bilaterally, targeting the near eye for -0.75 to -1.00 D will achieve reading vision without correction. Alternatively, patients may benefit from the placement of a monofocal IOL in their distance eye and an accommodating IOL with myopic defocus for intermediate and near vision in their contralateral eye.
FINANCIAL CONCERNS
In 2004, an estimated 1.04 billion people had presbyopia, but nearly half of them did not wear presbyopic correction, primarily in developing countries. Cataract surgery using pseudophakic monovision with monofocal IOLs is a cost-effective option to alleviate the burden of presbyopia.22
For patients with high cylindrical errors, a long-term cost analysis showed that toric IOLs were more cost-effective than conventional IOLs, because the former reduced patients’ postoperative need for spectacles and contact lenses.24 When implanting toric IOLs or toric accommodating IOLs, it therefore makes sense for surgeons to consider a monovision approach so as to reduce patients’ dependence on glasses and contact lenses.
In a 2008 study, 80% of all patients were willing to pay at least $5 per day, or $1,825 or more annually, to be free of spectacles.25 Nevertheless, the 2014 ASCRS survey found that presbyopia-correcting IOLs were being used in only 7% of cataract surgeries.12 Pseudophakic monovision can help to bridge the gap between patients’ desires, their finances, and the limitations of technology.
The economic gain of using presbyopia-correcting IOLs compensates the surgeon for the increased pre- and postoperative planning, testing, and counseling. Similar perioperative management and excellent surgical technique are required for success with presbyopia-correcting IOLs and for pseudophakic monovision. Although surgeons cannot bill for monovision itself, the use of noncovered services such as limbal relaxing incisions and adjunctive laser vision correction has allowed many surgeons to offer monovision as an effective part of their refractive packages or in conjunction with toric or accommodating IOLs.
CONCLUSION
Cataract and refractive lens exchange surgery offers patients an opportunity for improved visual function and decreased dependence on spectacles and contact lenses. Pseudophakic monovision is a common and effective strategy. Low levels of anisometropia can correct presbyopia without markedly impairing binocular function. Patients should be educated about the benefits and limitations of this approach, which is easily reversible with a pair of glasses or contact lenses. n
1. Josephson JE, Erickson P, Back A, et al. Monovision. J Am Optom Assoc. 1990;61:820-826.
2. Jain S, Arora I, Azar DT. Success of monovision in presbyopes: review of the literature and potential applications to refractive surgery. Surv Ophthalmol. 1996:40:491-499.
3. Wright KW, Guemes A, Kapadia MS, Wilson SE. Binocular function and patient satisfaction after monovision induced by myopic photorefractive keratectomy. J Cataract Refract Surg. 1999;25:177-182.
4. Jain S, Ou R, Azar DT. Monovision outcomes in presbyopic individuals after refractive surgery. Ophthalmology. 2001;108(8):1430-1433.
5. Goldberg DB. Laser in situ keratomileusis monovision. J Cataract Refract Surg. 2001;27:1449-1455.
6. Boerner, CF, Thrasher BH. Results of monovision correction in bilateral pseudophakes. Am Intra-Ocular Implant Soc J. 1984;10:49-50.
7. Handa T, Mukuno K, Uozato H, et al. Ocular dominance and patient satisfaction after monovision induced by intraocular lens implantation. J Cataract Refract Surg. 2004;30:769-774.
8. Ito M, Shimizu K, Amano R, Handa T. Assessment of visual performance in pseudophakic monovision. J Cataract Refract Surg. 2009;35:710-714.
9. Finkelman YM, Ng JQ, Barrett GD. Patient satisfaction and visual function after pseudophakic monovision. J Cataract Refract Surg. 2009;35:998-1002.
10. Greenbaum S. Monovision pseudophakia. J Cataract Refract Surg. 2002;28:1439-1443.
11. Leaming DV. Practice styles and preferences of ASCRS members-2003 survey. J Cataract Refract Surg. 2004;30:892-900.
12. Global Trends in Ophthalmology and the American Society of Cataract and Refractive Surgery. ASCRS Clinical Survey 2014. Published 2014. http://www.eyeworld.org/supplements/2014_ASCRS_clinical_survey.pdf. Accessed August 19, 2015.
13. Maxwell WA, Cionni RJ, Lehmann RP, Modi SS. Functional outcomes after bilateral implantation of apodized diffractive aspheric acrylic intraocular lenses with a +3.0 or +4.0 diopter addition power: randomized multicenter clinical study. J Cataract Refract Surg. 2009;35:2054-2061.
14. Packer M, Chu YR, Waltz KL, et al. Evaluation of the aspheric Tecnis multifocal intraocular lens: one-year results from the first cohort of the Food and Drug Administration clinical trial. Am J Ophthalmol. 2010;149:577-584.
15. Wilkins MR, Allan BD, Rubin GS, et al. Randomized trial of multifocal intraocular lenses versus monovision after bilateral cataract surgery. Ophthalmology. 2013;120:2449-2455.
16. Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2012;9:CD003169.
17. Xiao J, Jiang C, Zhang M. Pseudophakic monovision is an important surgical approach to being spectacle-free. Indian J Ophthalmol. 2011;59(6):481-485.
18. Hayashi K, Ogawa S, Manabe S, Yoshimua K. Binocular visual function of modified pseudophakic monovision. Am J Ophthalmol. 2015;159(2):232-240.
19. Maloney WF. Presbyopia success depends on comprehensive preop evaluation. Ocular Surgery News US Edition. August 1, 2005. http://bit.ly/1LhqMxJ. Accessed July 1, 2015.
20. Naeser K, Hjortdal J. Optimal refraction with monofocal intraocular lenses: no beneficial astigmatism. Acta Ophthalmologica. 2011;89(2):111-115.
21. Maloney WF. Pseudophakic monovision, mixing variable focal lengths. Cataract & Refractive Surgery Today. August 2007;7(8):59-61. http://crstoday.com/2007/08/CRST0807_07.php. Accessed August 17, 2015.
22. AAO Refractive Refractive Management/Intervention PPP Panel, Hoskins Center for Quality Eye Care. Preferred Practice Pattern Guidelines: Refractive Errors & Refractive Surgery PPP-2013. http://bit.ly/1WzQ7Gw. Accessed August 17, 2015.
23. US Food and Drug Administration. Ophthalmic Device Panel of the Medical Devices Advisory Committee Meeting Announcement. Appendix F: Literature Review on Accommodative Assessments of the Crystalens Accommodative IOL. April 8, 2013. http://www.fda.gov/AdvisoryCommittees/ucm340995.htm. Accessed July 1, 2015.
24. Pineda R, Denevich S, Lee WC, et al. Economic evaluation of toric intraocular lens: a short- and long-term decision analytic model. Arch Ophthalmol. 2010;128(7):834-840.
25. Maxwell WA, Waycaster CR, D’Souza AO, et al. A United States cost-benefit comparison of an apodized, diffractive, presbyopia-correcting, multifocal intraocular lens and a conventional monofocal lens. J Cataract Refract Surg. 2008;34(11):1855-1861.
Divya M. Varu, MD
• in private practice at Dell Laser Consultants, Austin, Texas
• dvaru@dellvision.com
• financial interest: none acknowledged