Case Presentation
A 64-year-old woman underwent laser cataract surgery with implantation of a Crystalens AO (Bausch + Lomb) in her left eye. The surgeon programmed a 5-mm capsulotomy (centered on the scanned capsule) and carefully polished the anterior capsule.
On postoperative day 1, the patient was thrilled with her UCVA: 20/20 for distance (plano refraction), 20/20 for intermediate, and 20/30 for near. She continued instilling an antibiotic for the first postoperative week and used steroid drops and a topical nonsteroidal anti-inflammatory drug (NSAID) for 4 weeks after surgery.
Six weeks postoperatively, the patient called the office to report a decrease in vision and was told to come in immediately. On examination, she had a distance UCVA of 20/40- and a -0.75 D refraction correcting to 20/20. The slit-lamp examination revealed coarse posterior capsular striae and a symmetrical, anteriorly vaulted Crystalens (Figure). The surgeon diagnosed impending Z syndrome and performed a central YAG capsulotomy of approximately 4.5 mm in diameter behind the optic. During the laser procedure, the IOL resumed a proper posteriorly vaulted position, and the patient’s visual acuity immediately returned to 20/20 and plano.
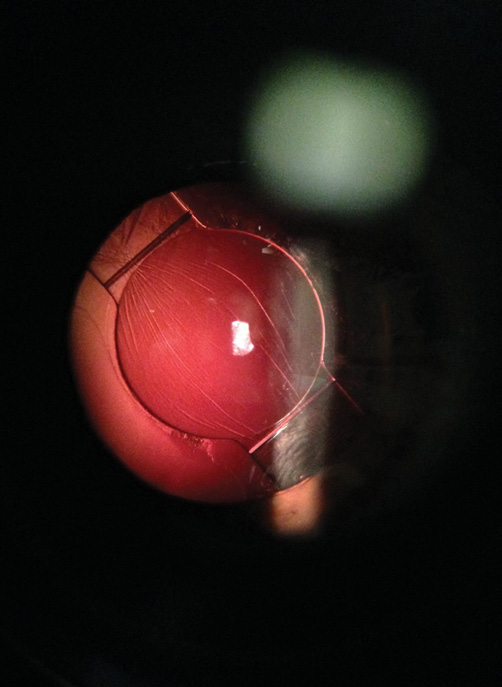
Figure. Coarse posterior capsular striae in the early postoperative period cause anterior vaulting of the Crystalens AO.
She was pleased until 2 weeks later, when she called back to say that her vision had just become very blurry. A repeat examination showed a full Z syndrome (3.00 D of induced refractive cylinder) with the inferior hinge of the IOL vaulting forward. Additional applications of YAG laser energy to the posterior capsule behind the vaulted hinge were not successful in resolving the Z syndrome.
How would you have handled this situation differently? What are the options now?
—Case prepared by Tal Raviv, MD.
DOUGLAS A. KATSEV, MD
This case demonstrates how to get the most from accommodating lenses. Effectively managing these patients justifies the increased out-of-pocket expenses for patients. The rewards of successful outcomes and a growing conversion rate can be realized with a few important surgical and postoperative steps. By consistently following them and never deviating from my protocol, I have been able to decrease problems in my practice.
The important steps of the procedure are
1. Ensure a tightly closed wound that does not leak. I sometimes place a suture to guarantee watertight incisions.
2. Rotate the IOL 360º or more to be sure that it is seated properly.
3. Clean and polish the capsule, especially the anterior capsule.
4. Follow up with patients 4 weeks postoperatively in order to detect any contraction of the bag early.
5. Have patients continue administering a steroid for a minimum of 4 weeks postoperatively. I frequently recommend they wear reading glasses for the first 2 weeks and perform cycloplegia (one drop of homatropine after the case) to relax early accommodation.
This case demonstrates an unusual event with accommodating lenses if all of the steps listed were followed. When capsular fibrosis occurs, it must be addressed. For this reason, I personally conduct a dilated examination of all patients 4 weeks postoperatively and will perform a YAG laser treatment for early capsular contraction. Usually, I perform a small central YAG capsulotomy and include the area of striae. I will also apply laser energy to the hinge if it shows signs of contraction of the bag locally. I usually do not connect treatment of the hinge with the central YAG procedure if both are needed. In this case, the initial result was great, but the bag has since contracted, with striae showing the area of tension. Applying YAG laser energy to this area should restore the precontraction results.
A conservative YAG treatment should solve excess cell growth. If the growth were aggressive, I would consider taking the patient back to the OR, where I would attempt to free the lens, rotate it 360º, and possibly place a capsular tension ring (CTR).
By taking the time to see patients a little more frequently during the first 90 days after surgery and addressing variations in the healing response, I have been able to increase my conversion rate to accommodating IOLs through word-of-mouth referrals.
ASIM PIRACHA, MD
The scanned capsular centration and 5-mm-diameter laser setting, careful polishing of the anterior and posterior capsules, and early YAG laser treatment for posterior capsular opacification and contraction show that the surgeon did everything appropriately to achieve excellent outcomes with this lens implant. Unfortunately, capsular contraction continued, and further capsulotomies posterior to both haptics did not resolve the issue.
To reduce the incidence of this complication, I have patients use both steroid and NSAID drops for 6 to 8 weeks postoperatively and a cycloplegic agent for 1 week after surgery. Additionally, at the conclusion of surgery, I rotate the IOL 360º to make sure that the haptics are fully within the equator of the capsular bag. At the initial YAG laser treatment in this case, I would not only have performed a posterior capsulotomy centrally (about 3 mm) but also separate capsulotomies posterior to each haptic and the fibrous bands to relax the capsular forces on the IOL.
At this point, one could enlarge the capsular openings posterior to the haptics and laser the fibrous bands/striae. If this were not successful and the patient desired better function, I would attempt to reposition the original Crystalens by placing a CTR, viscodissect the haptics off the anterior capsule, and place them in the equator of the capsule. If this procedure failed to resolve the Z syndrome, I would exchange the Crystalens by amputating the haptics as far distally as possible, perform a bimanual anterior vitrectomy, and then implant a three-piece acrylic monofocal IOL in the sulcus with optic capture to ensure proper centration and a better refractive outcome.
JONATHAN H. TALAMO, MD
In this case, performing a YAG laser posterior capsulotomy behind the optic was reasonable. The previously normal position of the IOL and the presence of vertical, radiating, posterior capsular striae emanating from a focal location along the inferior hinge of the IOL, however, suggested that asymmetric contractile forces were present elsewhere within the capsular bag that could cause a full-blown Z syndrome if left untreated.
If the anterior vaulting was severe, I would have taken the patient back to the OR before any laser treatment, attempted to free up the IOL within the capsular bag using viscodissection, and rotated the lens to a different axis. In that way, I would have broken adhesions that had formed, redistributed haptic-driven forces within the capsular bag, and ensured appropriate haptic footplate positioning within the fornix of the bag. I would then have placed a CTR. If these measures were unsuccessful, I would have performed an IOL exchange using a single-piece, monofocal, acrylic IOL. I would have amputated the haptics of the Crystalens at the hinge, left them in place if they were fibrosed into the bag, and positioned the three-piece IOL in the ciliary sulcus. After IOL repositioning, I would have injected triamcinolone and had the patient continue steroid and NSAID therapy for a minimum of 6 weeks.
Once a large posterior capsulotomy is present (as in this case), attempts to manipulate the IOL are more risky, so there is less to lose from additional laser treatment. Using the YAG laser, I would create radial relaxing incisions in the anterior capsule on either side of the superior hinge with the goal of releasing tension within the bag and allowing the superior hinge to flex forward and reduce the Z syndrome. If this treatment did not fix the problem, I would carefully examine the relationship of the IOL and anterior capsule to identify adhesions of the anterior capsule to the inferior IOL haptic complex and apply focal laser treatment to release them. If I did not think that anterior capsular adhesions to the inferior haptic were present and if treatment of the superior capsule were unsuccessful, I would perform an IOL exchange as described earlier, likely in combination with a bimanual anterior vitrectomy using either a limbal or pars plana approach.
JEFFREY WHITMAN, MD
I have really changed my approach to Crystalens implants that are poorly positioned after surgery. First of all, I instruct patients to use steroids for a minimum of 8 weeks postoperatively, because I have found that many of the problems related to fibrosis occur between 3 and 6 weeks after surgery. In this case, it would be helpful to know the axial length and power of the lens implanted, as they might have prompted me to insert a CTR at the time of surgery (long or short eyes). It is worth noting that the action area of the lens is actually the orange polyamide loops at the end of the haptics. They are designed to begin fibrosing into the equator of the bag after 3 to 4 weeks (so there will be a fixed pivot area for the lens).
I also dilate the pupil 4 weeks postoperatively to see if there are striae or asymmetrical fibrosis. If I observe either and the lens is still well positioned, I YAG the central posterior capsule and under the hinge-haptic area if dense, whitish fibrosis is noted. This single action has greatly reduced my rate of fibrosis syndromes. If, however, significant malpositioning of the IOL is inducing myopia, hyperopia, or more than 0.75 D of lens-induced astigmatism, I always reoperate rather than perform a YAG treatment for two reasons. First, I have found the failure rate of YAG treatment to be high in these eyes. Second, once the procedure is done, the options are very limited. When I operate, I viscodissect the bag open, rotate the lens at least 3 to 6 clock hours, and insert a CTR to help expand the bag. I then YAG the central capsule and any dense fibrosis over the haptic-hinge areas that can cause the bag to “close up” again. This has been my most successful plan for the treatment of severe Z syndrome, vaulting, etc.
Because the surgeon in this case proceeded with a YAG capsulotomy first, the capsule is now open. If feeling really brave, he or she can attempt viscodissection and use microinstruments to try to break the areas of fibrosis near the polyamide loops, but a vitrectomy is almost certain. Usually, amputation of the lens just peripheral to the hinges is necessary, and the optic-stump portion is removed, leaving the haptic remnants. I strongly recommend not sacrificing the capsular bag in an effort to get out the entire lens. The surgeon can then place his or her favorite three-piece IOL in the sulcus (a Tecnis Multifocal lens [Abbott Medical Optics] could even be considered). n
Section Editor Lisa Brothers Arbisser, MD
• emeritus position at Eye Surgeons Associates, the Iowa and Illinois Quad Cities
• adjunct associate professor, John A. Moran Eye Center, University of Utah, Salt Lake City
Section Editor Tal Raviv, MD
• founder and director, Eye Center of New York
• clinical associate professor of ophthalmology, New York Eye and Ear Infirmary of Mount Sinai
• (212) 889-3550; talraviv@eyecenterofny.com; Twitter @TalRavivMD
Section Editor Audrey R. Talley Rostov, MD
• private practice with Northwest Eye Surgeons, Seattle
Douglas A. Katsev, MD
• in private practice at the Sansum Clinic in Santa Barbara, California
• (805) 681-8950; katsev@aol.com
• financial disclosure: consultant to and member of the speakers’ bureau for Bausch + Lomb
Asim Piracha, MD
• medical director, John-Kenyon Eye Center, Louisville, Kentucky
• assistant clinical professor of ophthalmology and visual sciences, University of Louisville School of Medicine, Kentucky
• (800) 342-5393; asimp@mac.com; Twitter @johnkenyonLASIK
• financial disclosure: member of the speakers’ bureaus of Abbott Medical Optics, Alcon, and Bausch + Lomb and a clinical investigator for Abbott Medical Optics and Ophtec
Jonathan H. Talamo, MD
• director of Massachusetts Eye and Ear Waltham
• associate professor of ophthalmology, part time, Harvard Medical School, Boston
• (781) 890-1023; jonathan_talamo@meei.harvard.edu
• financial disclosure: consultant to Abbott Medical Optics and Alcon
Jeffrey Whitman, MD
• president and chief surgeon, Key-Whitman Eye Center, Dallas
• (214) 754-0000
• financial disclosure: consultant to Alcon and consultant to as well as referral source for Bausch + Lomb, particularly regarding the Crystalens


