Approximately 60% of patients presenting for cataract surgery will have 1.00 D or less of corneal astigmatism.1 Many of them would like to have their cylinder corrected to achieve optimal visual quality. When deciding how to correct 1.00 D of astigmatism, surgeons must take several variables into consideration, including the axis of cylinder and the alignment of corneal, refractive, and posterior corneal cylinder. The goal is to leave the patient with as little residual astigmatism and refractive error as possible.
COMPLETE WORKUP
In these cases, I like to perform a complete ophthalmic workup, including refraction, topography, optical path difference scanning, and biometry (IOLMaster; Carl Zeiss Meditec). This information will assist me in deciding how best to correct 1.00 D of astigmatism for the individual patient. I will then use intraoperative tools such as the Verion Image Guided System (Alcon) and ORA System (Alcon WaveTec) to account for surgically induced astigmatism and posterior corneal cylinder to refine the astigmatic correction.
The axis of corneal cylinder is an important factor, because with-the-rule (WTR) cylinder in the corneal plane typically has a lesser refractive effect requiring less astigmatic correction compared with against-the-rule astigmatism.2 A device such as the OPD-Scan III (Marco) can be used to measure the effect of posterior corneal astigmatism. Nomograms such as the Baylor Koch nonomgram can be used to integrate posterior corneal astigmatism into surgical planning. This type of nomogram will correct less astigmatism WTR and more astigmatism against the rule than using anterior corneal power alone.
ADDITIONAL DATA TO CONSIDER
An additional data point to consider when planning astigmatic correction is the patient’s refraction. For example, a patient may have 1.00 D of corneal cylinder but 2.00 D in his or her manifest refraction. In that situation, I am likely to choose a toric lens. Conversely, another patient with the same 1.00 D of corneal cylinder may have 0.75 D in his or her manifest refraction. I would likely plan to use a limbal relaxing incision or create arcuate cuts with the laser.
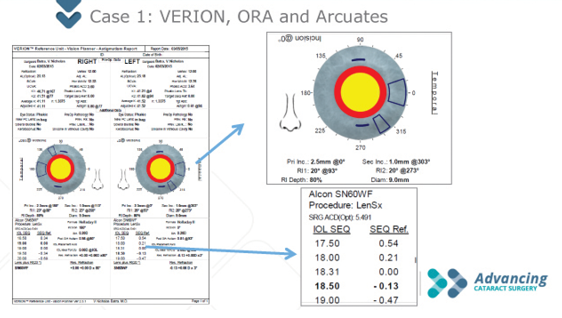
Figure 1. The author used the Verion to plan laser arcuate incisions to correct the patient’s astigmatism.
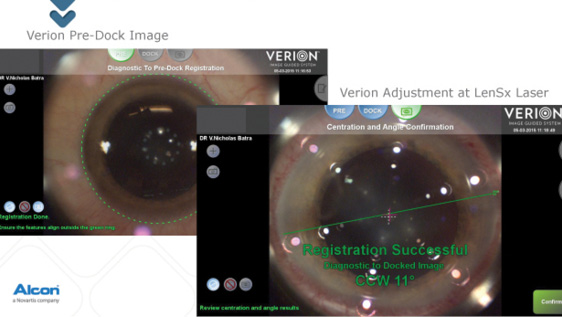
Figure 2. In this case, 11º of cyclotorsion was detected, and the limbal arcs were adjusted accordingly.
I used limbal relaxing incisions to correct approximately 1.00 D of corneal astigmatism in a patient with 0.98 D WTR corneal astigmatism in his right eye and 0.81 D in his left. I chose incisional surgery, because the patient had WTR astigmatism, and his refraction showed 0.75 D of astigmatism in both eyes, which would be less than what a low-powered toric lens would correct. In this case, I used the Verion to determine where to place femtosecond laser-created incisions to correct the patient’s astigmatism (Figure 1). A nice feature of the planner is that it allows me to toggle between correction of astigmatism with a toric IOL and limbal arcuate incisions. In this case, there was no residual cylinder with limbal arcuate incisions.
I take the information gathered from the image planner and enter it into the LenSx Laser (Alcon) to guide the astigmatic correction and correct for cyclotorsion. In the aforementioned case (Figure 2), 11º of cyclotorsion was detected, and the limbal arcs and incisions were adjusted accordingly.
Finally, once the cataract has been removed, I will use intraoperative aberrometry (ORA) to perform an aphakic refraction and check the result of the astigmatic correction with limbal arcuate incisions (Figure 3). In this case, I used the ORA to adjust the lens power from 19.50 to 20.00 D, and no additional astigmatic management was needed beyond the planned laser arcs.
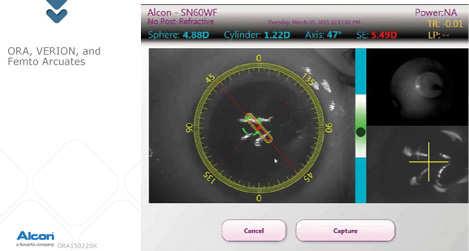
Figure 3. The author uses the ORA System to perform an aphakic refraction and check the result of the astigmatic correction with laser arcuate incisions.
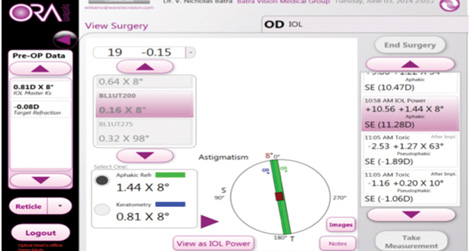
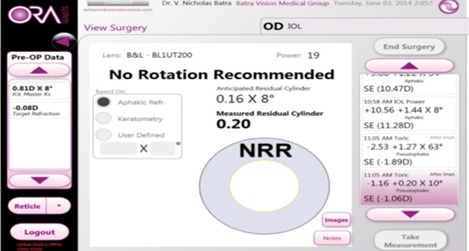
Figure 4. A Trulign BlU1T125 was selected based on the Trulign toric calculator, but the patient had 1.44 D of refractive astigmatism on intraoperative aberrometry. Thus, a BL1U200 was selected for the patient and spun to 8º.
In another case, the IOLMaster calculated 0.81 D of cylinder at 8º. The patient’s refraction showed 1.25 D of against-the-rule cylinder, so I elected to implant a Trulign BlU1T125 lens (Bausch + Lomb) based on the Trulign toric calculator. On intraoperative aberrometry, the patient had 1.44 D of refractive astigmatism, so I selected a BL1U200 for the patient and spun it to 8º (Figures 4). In this case, I used a toric lens with a larger astigmatic correction based on readings with the ORA. Postoperatively, the patient had less than 0.25 D of residual cylinder.
CONCLUSION
Both limbal relaxing incisions/laser arcuate incisions and toric lenses can be used to successfully treat 1.00 D of corneal astigmatism. The keys are verifying the axis of astigmatism, checking the refraction in comparison to the topographic astigmatism, accounting for posterior corneal cylinder, and then planning the astigmatic correction. Once the plan is created, I find it is important to adjust for cyclotorison and to use intraoperative aberrrometry to refine the astigmatic correction. In the end, the patients’ refractive targets can be achieved by combining the technologies mentioned herein. n
1. Miyake T, Kamiya K, Amano R, Shimizu K. Corneal astigmatism before cataract surgery [in Japanese]. Nihon Ganka Gakkai Zasshi. 2011;115(5):447-453.
2. Koch DD, Jenkins RB, Weikert MP, et al. Correcting astigmatism with toric intraocular lenses: effect of posterior corneal astigmatism. J Cataract Refract Surg. 2013;39(12):1803-1809.
V. Nicholas Batra, MD
• medical director of the Batra Vision Medical Group, San Leandro, California
• drbatra@batravision.com
• financial disclosure: consultant to Abbott Medical Optics, Alcon, Alcon WaveTec, and Bausch + Lomb


