Toric IOLs, although growing as a category, remain underutilized. This is likely due in part to the reluctance of patients to pay out of pocket for refractive cataract surgery (or surgeons’ reluctance to ask them to pay). It may also be related to surgeons’ concerns about having the right technology to succeed with toric IOLs.
Advanced tools such as intraoperative aberrometry and surgical guidance systems are certainly useful and may be a worthwhile investment for the refractive cataract surgeon who wants to further refine his or her outcomes. I would argue, however, that surgeons can and should get started with toric IOLs even if they do not have access to these expensive devices. With just a minimal investment in technology, toric IOLs can have a big impact on astigmatic patients.
Only three steps in toric IOL surgery differ from cataract surgery with a spherical lens: (1) measuring the corneal astigmatism as accurately as possible preoperatively, (2) marking the axis, and (3) placing the lens on the correct axis. Fortunately, all of these steps are either being used now by cataract surgeons or are easy and well within their capabilities.
MEASURING ACCURATELY
The first challenge is determining how much astigmatism needs to be corrected. This means isolating the corneal astigmatism from the lenticular component. Corneal astigmatism tends to be overestimated in eyes that have with-the-rule astigmatism and underestimated in those with against-the-rule astigmatism due to the contributions of the posterior corneal curvature.1
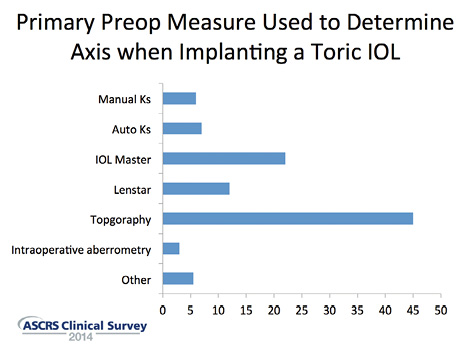
Figure 1. The American Society of Cataract and Refractive Surgery (ASCRS) Clinical Trends Survey suggests that most surgeons choose the axis based on topography.
There are multiple ways to measure corneal astigmatism, including manual keratometry, autorefractor keratometry readings (Ks), optical biometry with the IOLMaster (Carl Zeiss Meditec) or Lenstar (Haag-Streit), corneal topography, and anterior segment tomography with a device like the Pentacam Comprehensive Eye Scanner (Oculus) or Visante OCT (Carl Zeiss Meditec). There is no single right way to measure, but it is important to obtain multiple measurements for comparison and to try to bring them into reasonably close alignment.
The most recent ASCRS Clinical Trends Survey suggests that there is significant variation in which preoperative measurement surgeons trust most, with the largest group choosing the axis based on topography (Figure 1).2 I also use topography for my axis, but I will rely on Ks from the IOLMaster or Lenstar for the magnitude of astigmatism. Topography is also important to confirm the astigmatism is regular and not irregular such as from keratoconus.
When there is significant disagreement among various sources of measurement, it is important to figure out why. If one measurement seems “off” compared to the others, I repeat it. If I am getting five different sets of Ks, there may be ocular surface problems. Addressing dry eye disease and other ocular surface issues such as blepharitis, anterior basement membrane dystrophy, pterygia, or Salzmann nodular degeneration is important in any cataract surgery procedure but doubly so when depending on accurate keratometry to correctly place the right toric IOL.
Watch it Now
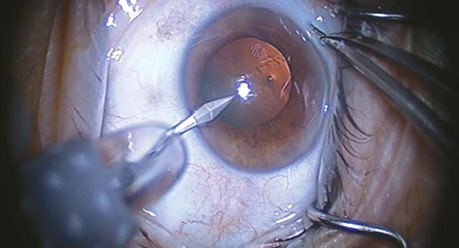
Figure 2. Dr. Mah demonstrates his intraoperative marking technique and alignment of a toric IOL (eyetube.net/?v=apevq).
Once the keratometry and axis are determined, each toric IOL manufacturer has an online toric calculator that is very easy to use and will help surgeons choose the correct IOL, axis for the IOL and incision, and final refractive outcome prediction.
MARKING AND ALIGNMENT
Marking and alignment are crucial (Figure 2). The change in the patient’s position from the slit lamp to the OR bed can create an unpredictable degree of excyclorotation. On average, the eye rotates about 4º when patients go from prone to supine, but 8% of eyes rotate more than 10º.3 For each degree of malrotation, there is a 3.3% loss of effect of the toric IOL power.4 The point of a significant loss of effect, especially with a higher powered toric lens, is quickly reached.
The methods that ASCRS members use to align the lens with the preoperative axis of astigmatism vary widely (Figure 3). The percentage using intraoperative wavefront aberrometry or digital image registration to help align a toric lens is quite small: only about 5% subscribe to each of these methods. The percentage of surgeons who say they either do not mark at all (6%) or rely on ink marking at the slit lamp without any additional intraoperative axial marking tools (31%) is surprisingly high.
Not marking the eye at all is quite risky. Using vessels in the eye or other markers for simple visual alignment is not reliable enough for accurate placement of a toric IOL, and making only preoperative marks at the major axes without marking the exact IOL axis of placement at some point may not be sufficient, either, because it is rare that the IOL needs to be placed at exactly 90º or 180º. There are a number of techniques for increasing the accuracy of marking, including one-step inkless markers, self-inking markers, dot cautery, degree gauges that attach to the slit lamp, marking systems with levelers, and placement of Nd:YAG or femtosecond laser pulses on the cornea. Perhaps the simplest place to start is with a radial corneal marker. When I first began implanting toric IOLs, I used an old limbal relaxing incision marker, but there are many inexpensive corneal markers available that can place a mark at the exact location, which is predicted to correct the patient’s astigmatism.
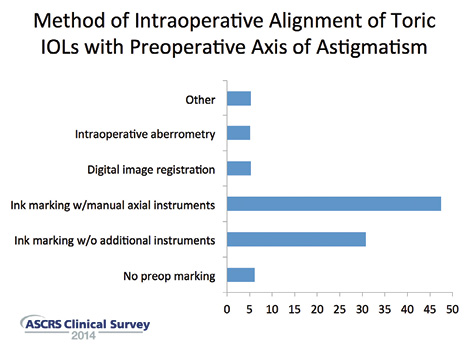
Figure 3. ASCRS members use a wide variety of approaches to align the lens with the preoperative axis of astigmatism.
GOING STEP BY STEP
The ophthalmologist instills a couple of drops of proparacaine. Just prior to surgery, with the patient sitting up at a slit lamp, the surgeon should ask him or her to “look at my ear but beyond it.” In my practice, we have actually placed a photograph on the back wall as a focal point for patients. Accommodation should be avoided because it induces excyclotorsion. Using a fine-tipped marking pen, the surgeon carefully marks 6, 3, and 9 o’clock (or 90º and 180º from the 6-o’clock mark). The eye should be relatively dry before marking, because a fat-tipped marker on a wet eye can make a very wide, imprecise mark from the ink’s bleeding.
In the OR, with the patient lying down, the surgeon preps and drapes as normal for cataract surgery. Before instilling any drops, the ophthalmologist aligns an axial corneal marker with the 90º and 180º marks and then finds the exact axis of astigmatism. The axis and intended incision location are marked. After phacoemulsification, the IOL is simply rotated in the bag to align it with the corneal axis marks. Finally, making sure to remove all of the viscoelastic from the eye is important for routine cataract surgery but even more critical for toric implants, because having significant contact with the capsule, both anterior and posterior, will improve stability and decrease possible rotation.
These simple steps should be enough to ensure good results and high satisfaction among toric IOL patients.
Initially, surgeons may want to start with the toric version of the spherical IOL platform with which they are most comfortable. Doing so will ensure already personalized A-constants and familiarity with the injector system. After the surgeon gains some experience with toric IOLs, it makes sense for him or her to try all of the available toric options and to consider factors such as rotational stability, contrast sensitivity, chromatic and spherical aberration correction, yellow chromophore, and the propensity for glistenings or other characteristics when choosing a toric IOL.
TAKING THE NEXT STEP
Eventually, many surgeons find that they want to do more to close the gap between good outcomes and nearly perfect ones. It is a small gap, and each new technology will offer only incremental gains.
A number of surgical guidance systems are now integrated with phaco machines, femtosecond lasers, and/or operating microscopes, including the Cassini TrueVision 3D system (iOptics/TrueVision), Callisto (Carl Zeiss Meditec), Verion (Alcon), and Cirle Surgical Navigation System, recently licensed to Bausch + Lomb (not yet commercially available). Despite differences, all of these devices help surgeons better register or align a toric IOL to the preoperative data, in many cases by projecting a digital overlay right through the operating microscope so that the need for marking is reduced or eliminated and accuracy enhanced.
Intraoperative aberrometry using the ORA System with VerifEye (Alcon WaveTec) or the new Holos IntraOp (Clarity Medical Systems; limited introduction for clinical use took place in early 2014, and full commercial release is anticipated in the second half of this year) goes a step beyond that to actually measure the astigmatism in the aphakic eye, after removal of the crystalline lens, and to facilitate alignment to optimize the correction.
These technologies represent opportunities to refine the toric IOL procedure, but the lack of them should not be viewed by surgeons as a barrier to their adoption of toric IOLs. These lenses can confer great benefits on astigmatic patients. n
1. Koch DD, Jenkins RB, Weiker MP, et al. Correcting astigmatism with toric intraocular lenses: effect of posterior corneal astigmatism. J Cataract Refract Surg. 2013;39(12):1803-1809.
2. ASCRS Clinical Trends Survey 2014. Survey overview available online at: http://eyeworld.org/supplements/2014_ASCRS_clinical_survey.pdf. Accessed April 10, 2015.
3. Swami AU, Steinert RF, Osborne WE, White AA. Rotational malposition during laser in situ keratomileusis. Am J Ophthalmol. 2002;133:561-562.
4. Ma JJ, Tseng SS. Effects of steep meridian incision on corneal astigmatism in phacoemulsification cataract surgery. J Cataract Refract Surg. 2012;38(4):666-671.
Francis Mah, MD
• member of the ASCRS Corneal Clinical Committee and the FDA Committee
• director of cornea and external disease and codirector of refractive surgery at Scripps Clinic Medical Group, La Jolla, California
• mah.francis@scrippshealth.org
• financial disclosure: consultant to Alcon, Abbott Medical Optics, and Bausch + Lomb/Valeant Pharmaceuticals


