Patients today expect 20/20 vision or better after LASIK eye surgery. Actually, that is no longer good enough; they also implicitly demand high-quality vision. Twenty years ago, LASIK delivered outcomes comparable to wearing soft contact lenses, but it could not compete with the vision quality afforded by gas permeable contact lenses. Since the advent and evolution of wavefront-guided laser technology, my colleagues and I at our practice have been able to consistently produce the quality of vision wanted by nearly every individual who walks through our doors.
In the infancy of wavefront-guided treatments, there was an expectation of “super” vision of incredible clarity. Unfortunately, the technology could not deliver, and the industry turned to wavefront-optimized lasers. The latter subsequently reached its maximum potential, while wavefront-guided technology continued to evolve. It is high time to take stock of where the treatments were versus where they are today.
GUIDED VERSUS OPTIMIZED
There are key differences between wavefront-guided and wavefront-optimized laser technologies. Conventional LASIK sets the basis for comparison. It relies on the refraction's results and the patient's preference when asked to compare corrective lens options during an examination. The resulting prescription is entered into the laser machine, and a theoretical lenticular pattern is used for treatment. This is the standard pattern used for all individuals bearing the same prescription and is also the method used in making glasses and contact lenses.
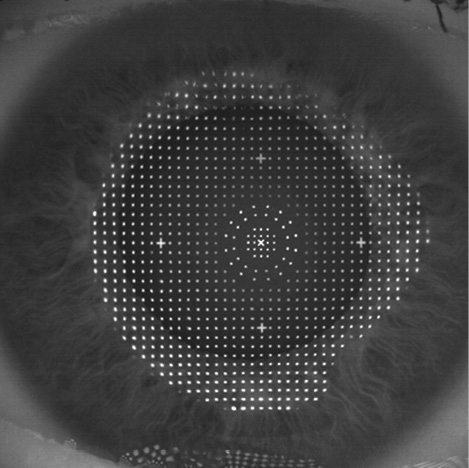
Figure 1. The iDesign software (Abbott Medical Optics) divides the eye surface into 1,000 squares (one-billionth of an inch tolerances) on a grid pattern and calculates the number of laser pulses to apply to each square to create a focused light ray that penetrates through each part of the cornea and pupil to focus perfectly on the fovea.
Wavefront-guided technology relies on a very precise method of optical measurement. By shining an infrared laser light into the eye, wavefront-guided technology can take the distorted light wave produced on its way back out and measure how the eye's optical system affected the light. The software then divides the eye's surface into 1,000 squares (one-billionth of an inch tolerances) on a grid pattern and calculates the number of laser pulses to apply to each square to create a focused light ray that penetrates through each part of the cornea and pupil to focus perfectly on the fovea (Figure 1). Wavefront-guided lasers target zero spherical aberration, and the goal is to reduce all higher-order aberrations.
This is not a basic spherical/cylindrical lower-order-aberration correction but rather an entirely different formula resulting in a highly customized visual result. In North America, wavefront-guided systems such as the Visx CustomVue (Abbott Medical Optics) and the Schwind Amaris (Schwind eye-tech solutions; available in Canada) have a reputation for producing exceptional results.
Wavefront-optimized LASIK is not necessarily comparable to the wavefront-guided procedure. The former is more accurately described as modified conventional LASIK. Just like standard LASIK, optimized laser treatment depends on the prescribed sphere and cylinder based on the patient's input; adjustments taking into consideration measured spherical or higher-order aberrations are not addressed. Optimized simply means “not intended to induce spherical aberration.” In fact, very few patients have zero spherical aberrations, especially those older than 40 years of age. With wavefront-guided LASIK, the goal is to reduce all higher-order aberrations. As previously stated, the spherical aberration target is zero.
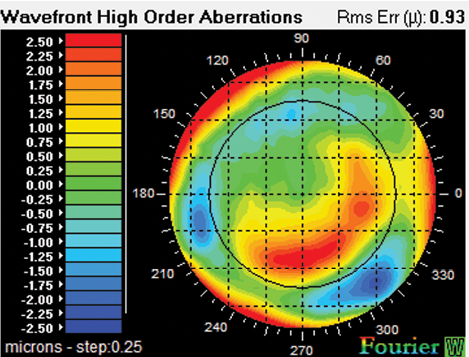
Figure 2. Fourier reconstruction combined with Hartmann- Shack technology provides wavefront-derived refraction, wavefront aberrometry, pupillometry, full-gradient corneal topography, and keratometry.
What differentiates wavefront-optimized LASIK from standard LASIK is the enhanced software developed to account for wavefront modeling and theory. This improves outcomes and reduces the occurrence of higher-order spherical aberrations when compared to standard LASIK. Both wavefront-optimized and wavefront-guided procedures administer extra pulses in the periphery of the laser ablation area to manage the LASIK-induced spherical aberration. Wavefront-optimized technology applies the same number of peripheral pulses for every patient with the same prescription, which effectively reduces induced spherical aberration commonly associated with standard LASIK. Wavefront-optimized LASIK does not, however, optimally treat patients with severe spherical aberration preoperatively, and it can worsen the night vision of patients with negative spherical aberration before surgery. Of course, surgeons can still produce excellent visual outcomes with this technology in the average patient, but I do not believe that the outcomes can compare to those achieved with a wavefront-guided laser.
HIGHER-ORDER ABERRATIONS
Treatment with wavefront-optimized lasers cannot address asymmetrical higher-order aberrations, such as coma or trefoil, and it thus may potentially worsen the quality of vision for a patient with negative spherical aberration. About 5% to 10% of my patients present with significant asymmetrical higher-order aberrations, and another 5% to 10% present with negative spherical aberration. These figures represent a significant number of patients who would not achieve the results they want with wavefront-optimized lasers, although this technology does a remarkably better job for these patients than conventional LASIK. Conversely, all patients obtain highly satisfactory results with wavefront-guided technology.
After adopting early wavefront technology in my practice, my outcomes noticeably improved. I established an effective system for managing nighttime glare and other problems in low light, but my success did not compare to the superior results I achieved on the Visx with iDesign and with my Amaris, which both have greater than 1,000 points of wavefront resolution (Figure 1). I perform 100% of my LASIK procedures with wavefront-guided technology and have been able to achieve results that I would never have thought possible.
PATIENT OPTIMIZATION
An important tool in analyzing complicated eyes is iDesign. This wavefront aberrometer uses Fourier reconstruction combined with Hartmann-Shack technology to provide a wavefront-derived refraction, wavefront aberrometry, pupillometry, full-gradient corneal topography, and keratometry (Figure 2). Full-gradient topography eliminates the gaps caused by skew rays and minimal sensitivity to the radial component of the gradient that currently exists with Placido disk topographers.
In addition to the role technology plays in producing superior outcomes, my protocol includes preoperative optimization of the ocular surface. Not only does this step improve the accuracy of wavefront and other measurements, but it also enhances postoperative healing and stability. I measure tear osmolarity with the TearLab Osmolarity System (TearLab) and complete dynamic tear film testing with the AcuTarget HD (AcuFocus). My staff and I manage patients using punctal plugs, prescription dry eye medications (topical steroids and Restasis [cyclosporine ophthalmic emulsion 0.05%; Allergan]), artificial tears, and meibomian gland dysfunction treatment when needed. This process may take weeks or even months, but refractive predictability and my long-term outcomes have definitely improved.
Approximately half of my potential LASIK patients are also contact lens wearers, the majority using soft contact lenses and motivated to have surgery because of reduced tolerance associated with dry eye disease. Preoperatively, I require patients to stay out of their contacts to allow the cornea to recover its natural shape. For soft lens wearers, 2 weeks is sufficient; gas permeable lens wearers must wait 1 month for each decade they wore contacts. I will also verify corneal stability between two topographical corneal maps taken 2 to 4 weeks apart before treatment. The eye is quite sensitive for picking up corneal aberrations, and it is imperative to allow the cornea to relax and go back to its natural shape. After following this protocol, more than 95% of my patients who have dry eyes with contacts will not experience postsurgical problems.
CONCLUSION
No longer is laser vision correction about taking the typical patient with mild to moderate myopia to 20/20 or 20/15. Nearly every laser can do that. The difference lies in how exquisitely surgeons can refine the patient's vision quality as well as the reproducibility and consistency of results. If the LASIK market is ever to grow again, surgeons must avoid performing standard LASIK. They must use advanced femtosecond lasers for flap creation and recognize that there is a small but significant segment of the population that definitely achieves superior results with wavefront-guided technology. It is true that the majority of patients will do equally well with wavefront-optimized technology. In my experience, the results are never superior to those achieved with wavefront-guided technology, and in a small percentage, they are inferior. I honestly believe that every patient deserves the quality of vision attained with today's state-of-the-art high-resolution wavefront-guided lasers. n
Jeffery J. Machat, MD, FRCSC, DABO
• founder and chief medical director of Crystal Clear Vision
in Toronto, Canada
• (416) 928-0777; jeff.machat@crystalclearvision.com
• financial disclosure: consultant to AcuFocus, Schwind, and
Ziemer