Case Presentation
A 44-year-old white woman with a history of keloids and systemic thyroid disease presently controlled with medication presents to you with a request for intervention 13 years after her LASIK surgery. She complains of decreased distance vision with asthenopic symptoms.
Prior to undergoing LASIK, the patient’s manifest refraction was -1.50 +2.50 × 110 OD and -1.25 +2.75 × 075 OS. Her preoperative keratometry readings were 42.37 @ 116/40.26 @ 025 OD and 43.12 @ 080/40.52 @ 170 OS. The surgeon created the flap with the Intralase FS laser (Abbott Medical Optics) and performed LASIK with the Autonomous laser on February 11, 2002. The procedure was uneventful.
One year postoperatively, the patient’s UCVA measured 20/25 OD and 20/20 OS. Her preoperative BCVA had been 20/30+2 OD and 20/20 OS. The patient was lost to follow-up until now.
She currently has a UCVA of 20/40+2 OD and 20/25-2 OS. Her manifest refraction measures -0.75 +0.75 ×110 = 20/20-2 OD and -0.25 +0.75 × 65 = 20/20 OS. Her cycloplegic refraction is +0.50 +0.75 × 110 = 20/25 OD and +0.75 +1.00 × 65 = 20/20 OS. Her wavefront refraction measures -0.01 +0.85 × 110 OD and +0.27 +1.06 × 072 OS (Figures 1 and 2). Root mean square (higher order) is 0.52 OD and 0.40 OS. An examination finds well-healed LASIK scars without other retinal or corneal abnormalities.
The patient desires a refractive enhancement for her left eye. What are her options?
—Case prepared by Karl G. Stonecipher, MD.
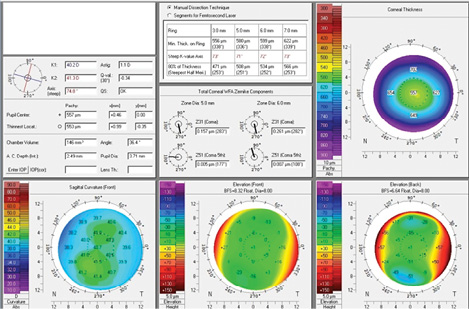
Figure 1. Diagnostic measurements with the Pentacam Comprehensive Eye Scanner (Oculus).
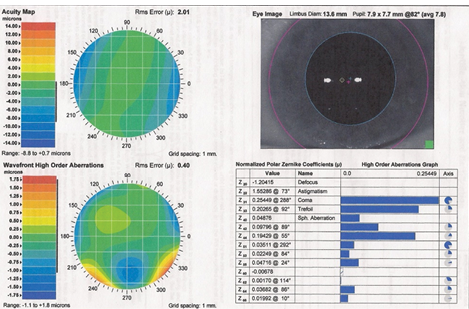
Figure 2. Diagnostic measurements with CustomVue (Abbott Medical Optics).
WILLIAM B. TRATTLER, MD
Patients who have undergone refractive surgery (PRK/LASIK) can return years later with a desire for an enhancement. A comprehensive evaluation is required to determine whether they will benefit from additional laser refractive surgery or whether alternative therapies are an option.
In this case, the patient had LASIK in her early 30s and is now in her 40s. Topography shows mild inferior steepening, but the axis of astigmatism is orthogonal. The wavefront examination shows coma, which is consistent with what one would expect when mild inferior steepening is noted. One of the challenges here is the 1.00 D difference between the manifest and cycloplegic refractions.
My first step would be a contact lens trial. I would determine which eye is dominant and then place a contact lens for reading on the patient’s nondominant eye. I would request that she spend a number of days with this setup to see if she were happy with her vision. If she were pleased, we could discuss a PRK enhancement for near in her nondominant eye.
If the patient were unhappy, we would discuss other potential therapies. One promising option under investigation, PRX-100 (Presbyopia Therapies), is a therapeutic eye drop that constricts the pupil without stimulating accommodation. Early results suggest the drug can improve patients’ near vision with minimal side effects. Another potential therapy under investigation is scleral expansion bands, which have the potential to restore accommodation.
Regardless of which direction the patient chooses to go, a thorough discussion of the potential risks versus benefits of the various options will be essential.
KEITH A. WALTER, MD
My first line of treatment in this case would be a contact lens trial. If the patient were happy with that modality, either full or part time, I would suggest she stay with that as her best option. If she really wanted intervention at this time, I would advise her that I would not do anything, because the risk is greater than the reward.
ROBERT J. WEINSTOCK, MD
Because of the patient’s 20/20-2 BCVA, I would encourage her to try other options prior to surgery. First, I would do everything possible to improve her ocular surface with punctal plugs, omega-3 supplements, and topical cyclosporine (Restasis; Allergan) as indicated. If her complaints persisted, as a final option, I would discuss with her a surface treatment using the Nidek EC-5000 CXII excimer laser system (Nidek). I would spend extra time discussing with the patient the issues of laser vision correction in someone with a history of keloids. n
Section Editor Alan N. Carlson, MD
• professor of ophthalmology and chief, corneal and refractive surgery, Duke University Eye Center, Durham, North Carolina
Section Editor Stephen Coleman, MD
• director of Coleman Vision, Albuquerque, New Mexico.
Section Editor Karl G. Stonecipher, MD
• director of refractive surgery, TLC in Greensboro, North Carolina
• (336) 274-2244; stonenc@aol.com
William B. Trattler, MD
• director of cornea at the Center for Excellence in Eye Care in Miami
• (305) 598-2020; wtrattler@earthlink.net; Twitter @wtrattler
• financial disclosure: consultant to and speaker for Abbott Medical Optics, recipient of research support from Refocus Group
Keith A. Walter, MD
• associate professor of ophthalmology, Wake Forest Baptist Medical Center, Winston-Salem, North Carolina
• (336) 716-4091; kwalter@wakehealth.edu
Robert J. Weinstock, MD
• director of cataract and refractive surgery, Eye Institute of West Florida, Largo, Florida
• rjweinstock@yahoo.com; Twitter @EyeInstituteWFl
• financial disclosure: consultant to Allergan


