
In my experience, presbyopes who are motivated to get rid of their reading glasses are overwhelmingly happy with a Kamra inlay (AcuFocus), and their results justify the time spent on postoperative management.
Mild corneal steepening over the inlay or minor changes in refraction are normal postoperative findings that generally do not require treatment. Healing time is typically 1 month, with patients gaining 3 lines of visual acuity by 1 week and an additional line by 1 month postoperatively. Minimizing surgical time may reduce edema and healing time.
Near and distance vision with the inlay is dependent on refractive error. Patients who do not achieve the target refraction of -0.75 ±0.25 D in the inlay eye and plano in the fellow eye may not have the UCVA they desire. Regression and the method of assessment can affect the postoperative refraction. Autorefraction is unreliable in an eye with an inlay; a midpoint refraction should be performed. Fluctuations in vision are usually due to dry eye and associated with poor compliance with the postoperative drop regimen.
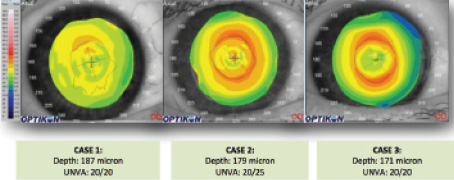
Figure 1. The presence of a red ring on topography can be influenced by the implant's depth. These three patients had their inlay implanted at different depths. The deeper implant has no ring, whereas the shallower implant has an obvious ring. Abbreviation: UNVA, uncorrected near visual acuity.
Pocket implantation, even in patients who also require LASIK, has simplified postoperative management. Global registry data show that the incidence of wound healing response has declined from 17% with the combined LASIK-Kamra procedure under a thick flap to 4% when the inlay is implanted in a corneal pocket (data on file with AcuFocus).
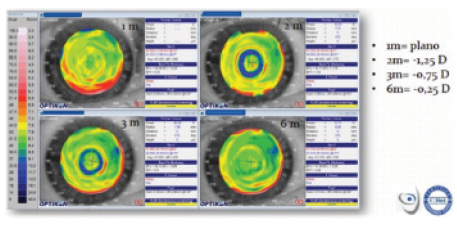
Figure 2. This patient had a good result at 1 month. At the 2- and 3-month visits, however, there appeared to be a myopic shift, and a blue ring was seen on the topographic axial map. Dry eye treatment resolved the problem.
look at the axial map
For the most accurate view of any areas of elevation on topography, surgeons should look at the axial map, rather than the instantaneous or tangential radius of curvature map. It is fairly common to see a red ring of mild, midperipheral steepening over the inlay. This is statistically significantly correlated with inlay's depth, time since surgery, and ablation type.1 In Figure 1, the red ring is most obvious in the eye with the shallowest implantation.
By itself, a red ring is of no consequence and does not require therapy. When a red ring is accompanied by central flattening, haze formation, and a hyperopic shift, however, I recommend corticosteroid treatment.
A blue ring or area of flattening over the inlay is also not necessarily cause for concern. In most cases, this is due to tear film irregularity, which can result in a myopic shift and central steepening. Aggressive ocular surface treatment will resolve the problem (Figure 2). When accompanied by corneal haze and stromal thinning noticeable on optical coherence tomography, one might consider removal, but I have never seen this. Nor has this been reported commercially. In fact, I have removed only one inlay out of 200, and that one was due to the patients dissatisfaction rather than a complication.
At a Glance
• Mild corneal steepening over the inlay or minor
changes in refraction are normal postoperative findings
that generally do not require treatment.
• Pocket implantation, even in patients who also require
LASIK, has simplified postoperative management.
• When postoperative refractive shifts occur, they are
related to changes in epithelial thickness rather than a
stromal response.
My recent optical coherence tomography studies suggest that, when postoperative refractive shifts occur, they are related to changes in epithelial thickness rather than a stromal response. Based on my experience, in the majority of eyes, appropriate management with topical steroids or dry eye therapies will reduce steepening and reverse a refractive shift so that patients achieve the target refractive result. n
1. Carones F. Assessment of the Kamra inlay using videokeratography and corneal OCT: 2-year results. Paper presented at: The ESCRS annual meeting; October 5-9, 2013; Amsterdam, Netherlands.
Francesco Carones, MD
• medical director, Centro Oftalmo-Chirurgico Carones, Milan,
Italy
• fcarones@carones.com
• financial disclosure: advisor to AcuFocus


