Centurion Vision System
By Brandon D. Ayres, MD
Alcon's latest phaco unit, the Centurion Vision System, represents 10 years of research and design and features numerous advances over its predecessor, the Infiniti Vision System. I have been using the new machine for approximately 9 months on several hundred cataracts and about
100 endothelial keratoplasty procedures. Overall, my experience has been very positive. It would be almost impossible to discuss each and every technological improvement, but this article mentions several.
FLUIDICS
The most significant improvement on earlier phaco units is the addition of active fluidics. Gone are the days of hanging a bottle of balanced salt solution from a pole. With the Centurion, the irrigating solution is placed between two bellows located in the body of the unit. Instead of adjusting the bottle height to account for fluid loss, surge, and aspiration flow rate, I simply select a target IOP. Once that level is reached, the Centurion uses an active feedback loop to maintain the IOP at the set level by adjusting the pressure the bellows place on the irrigating fluid bag (Figure 1).

Figure 1. The fluid management cartridge for the Centurion. Visible are the dual elastomer segments as well as the irrigation and vacuum sensors essential to the active fluidic feedback loop.
Figure 2. The Intrepid balanced tip. The unique tip configuration is designed to maximize torsional phaco energy.
Before I used the Centurion, I figured that the active fluidics was going to be a gimmick, but I could not have been more wrong. I immediately noticed the improvement in anterior chamber stability. Initially, I operated with an IOP of
55 mm Hg, but I have since increased the pressure to 65 mm Hg, which has further improved stability and allowed for more aggressive phaco settings. Greater anterior chamber stability is also evident during procedures such as Descemet stripping endothelial keratoplasty and suturing IOLs when I use an anterior chamber-maintaining cannula instead of the I/A or phaco handpiece.
PHACOEMULSIFICATION
The Infiniti was adapted to torsional phacoemulsification or Ozil Intelligent Phaco (Alcon). In contrast, the Centurion was designed to maximize torsional technology. The Intrepid balanced tip is a new design with several enhancements of the traditional Kelman tip (Figure 2). The new instrument has a double-bend design that delivers energy through the shaft of the needle to focus energy at the tip.
I was accustomed to the bend in the Kelman tip. It took two or three cases before I felt comfortable using the balanced tip, but the transition was pretty easy. The improved cutting efficiency of the balanced tip was evident, and at first, the speed of lens removal was unnerving. Overall, I have been able to lower my phaco and torsional settings without decreasing my ability to remove lens fragments. With the use of the balanced tip, I have noticed a significant reduction in cumulative dispersed energy, even in eyes with a dense cataract. At first glance, the modifications to the tip seem small, but the increased efficiency of lens removal is immediately noticeable.
PART OF THE WHOLE
The Centurion is not a standalone phaco machine but the centerpiece of a technology-driven OR. I liken the unit to the conductor of an orchestra. Through the foot pedal (which is finally wireless), the Centurion ties together the other components of Alcon's Cataract Refractive Suite. One of the most notable parts of this suite is the Verion Image Guided System, which consists of a registration unit that images the conjunctival, limbal, and iris architecture as well as reads keratometry. By adding axial length, ophthalmologists can complete all surgical planning on the unit.
I have found the Verion reference unit simple to use and have heard few complaints from my staff. The technology has made surgical planning easier and has increased my conversion rate to laser cataract surgery. The integration of Verion with the LenSx Laser (Alcon) is seamless. The Verion's display is viewed through the left ocular and can be turned on and off at my request. At first, I tried to operate with the display on all of the time but ultimately found it too distracting. Now, I turn it on only for IOL centration or toric IOL alignment. I have been centering multifocal IOLs on the preoperative undilated pupil with excellent success. Setup and control of the Verion unit on the microscope is the only time I hear my scrub nurse complain. It is an additional step that can confuse OR staff members who do not perform it regularly.
CONCLUSION
The Centurion is a state-of-the-art phaco machine. My only criticism is that it may be too customizable. So many variables can now be modified that it is easy to get lost in the operating system. I strongly recommend that, for their first several cases, new users have a surgical representative from Alcon who knows the system well help set up the machine. I now have several settings for soft and dense lenses that would have been impossible to develop without such assistance.
Stellaris Vision
Enhancement System
Cataract surgeons are discovering that their ability to deliver the improvements in surgical procedure and enhanced visual outcomes that the femtosecond laser promises depends, in part, on how well their phaco platform performs, particularly during removal of the laser-treated lens. Features that might have been a matter of preference a few years ago now really matter, because they either complement the laser procedure or add new challenges. I have found that the Stellaris Vision Enhancement System (Bausch + Lomb) offers several distinct advantages that support the success of my laser cataract cases.
MAINTAINING A STABLE CHAMBER WITH HIGH VACUUM
The ability to use high vacuum settings with exquisite control is probably the most important benefit of the Stellaris. Laser-treated lens fragments are more difficult to capture with the phaco and/or I/A tip, making high-vacuum aspiration the ideal approach to their removal and to cortical cleanup. Maximum control is critical, however, to avoid surges when the phaco and/or I/A tip is occluded and then suddenly clears.
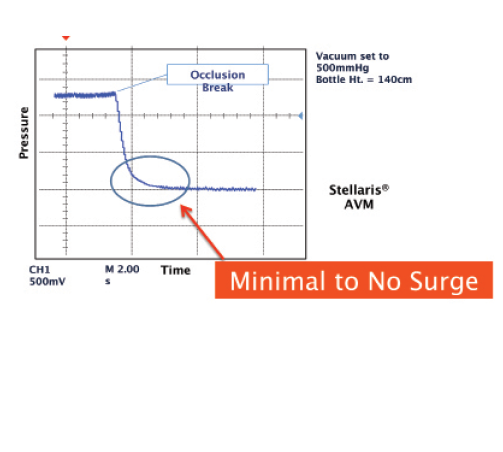
Figure 1. The Advanced Vacuum Module StableChamber Fluidics System minimizes surge with a 1.8-mm microincisional cataract surgery tip during high vacuum. Data on file with Bausch + Lomb.

Figure 2. The Stellaris PC.
Typically, I create a waffle-like pattern on the nucleus with the laser. I have found that small, floating fragments can be quite difficult to remove without high vacuum and a stable anterior chamber. The Stellaris enhances fluidics control under high vacuum with its unique StableChamber tubing. The system also allows me to choose among Digiflow pressurized infusion settings. All of these features give me precise control with high vacuum and ensure outstanding chamber stability throughout every procedure, whether I am performing traditional or microincisional cataract surgery. I prefer the latter for patients at risk of intraoperative floppy iris syndrome, and high vacuum settings would be risky in these cases without precise control. The anterior chamber stays deep during high vacuum, and with 1.8-mm microincisional surgery, iris prolapse is minimal or nonexistent in my experience (Figure 1). I have found my need for ancillary pupillary devices is confined mainly to patients with small pupils, not floppy irides.
The benefits of carefully controlled high vacuum extend to cortical cleanup, a step that many surgeons find to be more challenging with laser-treated lenses because of greater cortical adhesion to the capsular bag. Using a circumferential pattern to remove cortical material, I have not found this step to be any more difficult than in a conventional procedure.
MINIMIZING THE IMPACT OF PHACO POWER
Decreasing the amount of ultrasound power we put into the eye reduces corneal edema and improves immediate postoperative outcomes. Laser fragmentation of the lens, combined with high-vacuum aspiration, offers the best opportunity to lower phaco energy. In a routine cataract case, I do not need to sculpt and often only require a second or less of microburst-mode phacoemulsification. The Stellaris' 28.5-kHz six-crystal phaco handpiece lets me achieve low-energy, high-efficiency bursts of power. I find that the unit's Attune Energy Management System delivers consistent power, enhances “followability,” generates less heat, and increases phaco efficiency.
The yaw position on the wireless dual-linear foot pedal gives me linear control of ultrasound and aspiration, especially during epinuclear removal. The Stellaris allows aspiration of the epinuclear plate via the phaco tip with or without ultrasound, depending on the surgeon's preference. This unique feature further lowers the phaco energy delivered to the corneal endothelium.
IMPROVING EASE OF USE AND VERSATILITY FOR THE BUSY PRACTICE
Another benefit of the Stellaris is how well it fits in a busy cataract practice. Featuring streamlined and intuitive user interfaces, the unit has a compact footprint. Setup, including automated tubing priming and handpiece tuning, takes 3 minutes. This efficiency is optimized with the Stellaris PC, which supports cataract and vitreoretinal procedures on a single platform (Figure 2). Using one console in the ambulatory surgery center for both the anterior segment surgeon and the vitreoretinal surgeon reduces the amount of equipment needed as well as service and supply costs.
The only limitation of the Stellaris and other phaco platforms, in my opinion, is the lack of a true femtosecond setting to be used with any of the laser systems. Although I have great success with the Stellaris' microburst setting for extracting waffle-like nuclear fragments, this software setting was not originally developed for removing nuclear segments after laser fragmentation. Further refinement is needed to find the sweet spot for true phacoemulsification after laser fragmentation.
CONCLUSION
Just as I recognize potential synergies between the femtosecond laser and the phaco unit, I view the other tools I use as a comprehensive set that allows me to offer the highest quality of vision to my patients. Having the opportunity to correct astigmatism with laser arcuate incisions or with the Trulign Toric Posterior Chamber IOL (Bausch + Lomb), for example, allows me to tailor the cataract procedure to each patient's lifestyle and vision requirements.
I perform approximately 1,200 cataract surgeries each year and have been increasingly successful at educating patients about the advantages of femtosecond laser technology. My practice now has an 80% conversion rate for the procedure, a testament to its perceived value and the outcomes we have achieved. In light of patients' high expectations regarding their visual acuity after a premium procedure, I have come to appreciate the role that my phaco system plays in delivering the full promise of laser cataract surgery.
Whitestar Signature System
Phacoemulsification has gone back to the future since the advent of laser cataract surgery. Reversing a recent trend, larger-bore phaco needles are replacing smaller ones, and fluidics have returned as a major feature of modern machines.
The Whitestar Signature System with Fusion Fluidics (Abbott Medical Optics) is primed for this evolution, because it is the only unit on the market that carries two pumping systems (Figure 1). With both a peristaltic and a Venturi pump in a single cassette, the fluidics of choice are available to cataract surgeons with a tap of the foot pedal. Moreover, thanks to nonrepulsive transversal phaco technology, this machine is suited to anything from a laser-softened, prefragmented nucleus to a dense cataract.
FLUIDICS
Just as many cataract surgeons use two viscoelastics in one case so as to blend the best characteristics of a dispersive and a cohesive, Signature users such as myself can apply the best of both fluid pumps. The advanced peristaltic pump provides excellent “holdability” early in a case. For example, the peristaltic pump holds the lens securely to permit vertical or horizontal chopping. Similarly, after the laser-assisted steps of the cataract procedure, I can use the peristaltic pump to help break up the prefragmented segments. Tip occlusion is required to produce vacuum, and this is easily achieved early in the case when the lens is relatively immobilized.
In contrast, because a Venturi pump achieves vacuum immediately (in the cassette), it can be used to attract nuclear segments to the phaco tip without full occlusion. The Signature's Venturi pump has built-in sensors to safeguard against rapid fluctuations in flow. In fact, for most cases, I set vacuum to a maximum of 150 mm Hg. The benefits of a Venturi pump really shine in laser cases. Typically, I fragment the lens into small cubes with the laser, which decreases the need for phaco power. The small cubes make achieving occlusion more difficult in peristaltic mode, whereas Venturi fluidics magnetically vacuum up these free-floating pieces.

Figure 1. The Whitestar Signature Bausch + Lomb System with Fusion Fluidics.

Figure 2. The Ellips FX handpiece.
IRRIGATION AND ASPIRATION
A Venturi pump is also advantageous during I/A. Because full occlusion is not required, tags of cortex are easily drawn to the tip. For example, just getting the tip close to subincisional cortex allows its safe removal in virtually all my cases without my having to rely on curved tips or bimanual I/A.
I find that laser cataract surgery produces “stickier” cortex during I/A, probably due to difficulty in achieving a plane for cortical cleaving hydrodissection and to thermal effects sealing the cortex to the anterior capsule. Venturi fluidics, again, offer an advantage over peristaltic I/A in these cases.
PHACOEMULSIFICATION
The Signature's phaco handpiece is compatible with a straight or curved (Kelman-style) tip and with 19-, 20-, and 21-gauge tips (Figure 2). This versatility allows surgeons to follow their preferences in terms of technique and incision size.
For traditional cataract surgery, I prefer a curved tip. After the laser cataract procedure, however, because sculpting is unnecessary, I find a straight needle is easier to maneuver safely away from the posterior capsule and cornea. A 20-gauge needle allows for efficient evacuation of the fragmented cubes, which easily clear the lumen.
Through its combination of lateral and longitudinal motion into the phaco movement, transversal ultrasound is highly efficacious for removing all grades of nuclei. In laser cataract surgery, the quantity of phaco energy is reduced and sometimes eliminated. My goal, however, is not zero phacoemulsification so much as it is zero trouble and zero complications. Transversal ultrasound lets me remove the lens efficiently with less heat and lens repulsion.
I am creating a laser phaco setting on the Signature that will optimize the fluidics-driven mechanics. For these cases, I use a 20-gauge straight needle. I have two techniques, either a “femto flip” for soft lenses (and they are mostly soft after fragmentation) or a “femto chop” for dense lenses. In both instances, I use Venturi fluidics with vacuum set at 150 mm Hg (and a foot pedal yaw set up to boost vacuum to 300 mm Hg), increased foot position 2 excursion, and a transversal maximum power of 30.
I would like to see an evolution in the design of the traditional phaco tip. A sharp, beveled, metal tip is unnecessary for these cases. I look forward to new, round, blunt, nonbeveled designs that are more like I/A tips.
CONCLUSION
Being able to tap into both peristaltic and Venturi fluidics as well as the efficiency of transversal ultrasound gives the Signature system the versatility to handle all cataract grades and surgeons' techniques, whether for a traditional or a laser-assisted cataract procedure.n
Brandon D. Ayres, MD
• surgeon, Cornea Service, and codirector of the cornea fellowship,
Wills Eye Hospital, Philadelphia
• (484) 434-2700; bayres@willseye.org; Twitter @bfast33
• consultant to and speaker for Alcon
Mitchell A. Jackson, MD
• founder and CEO, Jacksoneye, Lake Villa, Illinois
• mjlaserdoc@msn.com; Twitter @djmjspin
• consultant to Bausch + Lomb and Lensar
Tal Raviv, MD
• founder and director, Eye Center of New York
• clinical associate professor of ophthalmology, New York Eye
and Ear Infirmary of Mount Sinai
• (212) 889-3550; talraviv@eyecenterofny.com
• consultant to Abbott Medical Optics and speaker for Bausch + Lomb


