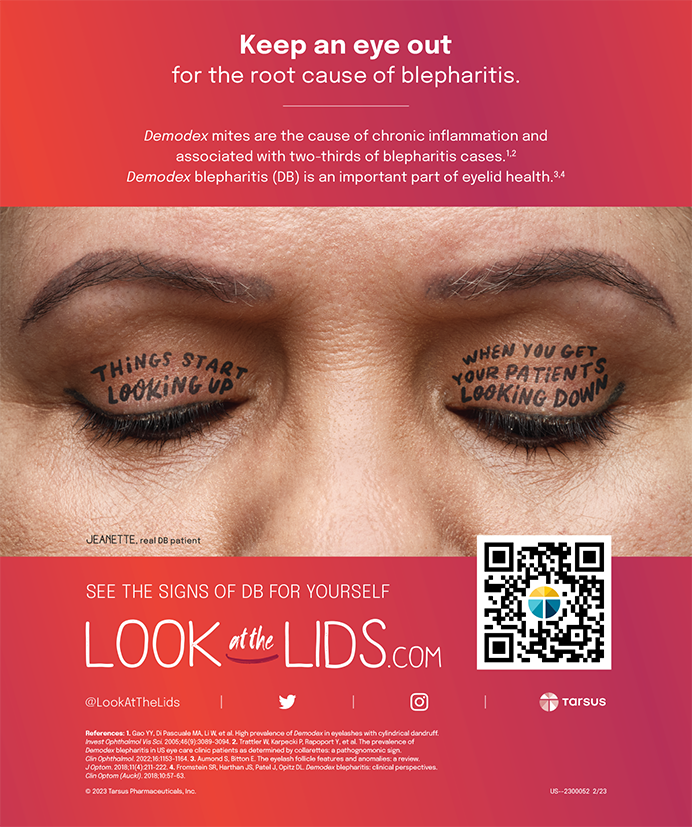
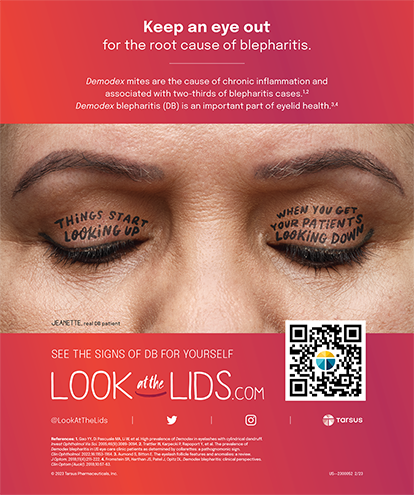
Technological advances in the diagnostic, surgical, and nonsurgical treatment of irregular astigmatism due to corneal scarring are encouraging. As concerned corneal refractive surgeons, we must continue to study and incorporate these advances to better care for our patients. This article will define the medical condition, incidence, etiology, diagnosis, and both surgical and nonsurgical treatment of irregular astigmatism with corneal scarring (Figure 1).
DEFINING THE TERMS
It is important that the surgeon have an excellent understanding of optics terminology. Astigmatism occurs when the curvature of the cornea (or lens) varies in different meridians.1 Regular astigmatism is produced when the steeper and flatter meridians are perpendicular to each other.2 Irregular astigmatism occurs when the orientation of the principal meridians changes from one point to another across the pupil, or when the amount of astigmatism changes from one point to another.1 Regular astigmatism is correctable using a cylindrical spectacle lens. The further distinction of irregular astigmatism includes regularly or irregularly irregular astigmatism and relates to the presence of pattern recognition on computerized topography. Irregularly irregular astigmatism is rough or uneven, and shows no recognizable pattern on topography.3
Corneal opacities occur when altered stromal keratocytes either (1) fail to produce certain chemical factors after infection, trauma, or surgery, or (2) form underlying disease or dystrophy. New collagen fibers become disorganized, scatter light, and result in a nontransparent scar. The location, size, texture, and depth of the corneal opacity are all critical to the patient's visual potential. By definition, some degree of irregular astigmatism is expected with any corneal opacity.
INCIDENCE
Research based on corneal topography suggests that approximately 40% of all naturally occurring astigmatism is irregular.3 A careful review of the literature fails to determine the total number of patients who suffer from lost BCVA secondary to irregular astigmatism from corneal opacities. It is possible, however, to determine the percentage of patients who undergo corneal transplantation for corneal opacification based on data from eye banks. Approximately 12% of all corneal transplants in the US in 1995 were due to corneal opacification, including corneal dystrophies, degenerations, trauma, and postinfection.4 In addition, a significant number of phototherapeutic keratectomies are performed to treat corneal scarring with associated irregular astigmatism.5
ETIOLOGY
Corneal opacities may arise as congenital lesions, dystrophies, or degenerations after viral, bacterial, fungal, or amoebic infections and as a result of surgery or other trauma. The list of corneal pathologies amenable to PTK is an excellent resource for the refractive surgeon.4 Understanding the pathophysiology of these entities enables researchers to establish specific treatment algorithms.
Patients who develop iatrogenic irregular astigmatism and corneal opacity after an elective procedure particularly concern all refractive surgeons, because the condition has been found after a variety of procedures, including RK, ALK, PRK, LASIK, and LASEK. Whether these patients suffer from intraoperative or postoperative complications, or abnormal healing, they represent a special subset that merits our greatest efforts. Fortunately, these complications are quite rare following procedures performed by skilled surgeons (Figure 2).6
DIAGNOSIS
Most of the tools necessary to diagnose irregular astigmatism in the presence of corneal scarring are readily available to all refractive surgeons. First, the physician must determine a good refraction (manifest and cycloplegic) for BCVA and document the presence and type of corneal scar during the slit-lamp examination. Photographic documentation and optical pachymetry may assist in delineating the extent of the corneal opacity.
Although retinoscopy may become a lost art, it is invaluable as a simple method for estimating the refractive state of the eye. Those familiar with the retinoscope recognize scissoring or undecipherable reflexes as the hallmarks of irregular astigmatism. Irregular mires on keratometry or even on applanation tonometry can often be identified in patients with irregular anterior corneal surfaces. Most refractive surgeons are familiar with the irregular patterns on corneal topography that denote irregular astigmatism. Software analysis, available in systems developed by Stephen D. Klyce, PhD, and Jack Holladay, MD, are readily available to assist the physician. The surgeon must be aware of irregularities of the tear film and posterior corneal changes, both of which may confuse the diagnosis.
Commonly, a hard contact lens overrefraction will improve the BCVA of a patient with irregular astigmatism. In fact, many patients with corneal dystrophies or other opacities have been successfully treated with these lenses, and gained excellent vision despite the cornea's appearance. Recent advances in wavefront technology greatly assist ophthalmologists in diagnosing and treating these particular corneas. By measuring higher-order aberrations, these devices help to precisely define irregular astigmatism. Also, excimer laser technologies allow surgeons to generate and apply treatment algorithms.
TREATMENT OPTIONS
Successfully treating patients with irregular astigmatism can be difficult and may, at times, frustrate both the surgeon and the patient. Those who suffer from significant corneal opacities with associated irregular astigmatism have historically benefited from a penetrating keratoplasty to replace the entire cornea or a lamellar keratoplasty to partially replace it. Complications associated with both techniques, however, are significant and must be explained to the patient. In particular, infection, rejection, glaucoma, interface scarring, irregular astigmatism, and prolonged visual recovery are concerns with these patients.
Spectacles
A small percentage of patients with minimal scarring and irregular astigmatism of low magnitude may benefit from spectacles featuring newer antireflective coatings and polarizing lenses. Although many patients suffering from this corneal condition do not find satisfaction with spectacles, this treatment is noninvasive and may thus warrant a trial.
Contact Lenses
Fitting contact lenses over a patient's corneal opacity with irregular astigmatism is an excellent treatment option and may either temporarily or permanently improve his BCVA. Carefully fitting an irregular astigmatism patient after he undergoes refractive surgery has proven successful;7 however, the extent of a patient's corneal scarring may affect the success of this nonsurgical technique.
Keratoplasty
Advances in microkeratomes have led to improvements in lamellar keratoplasty. New techniques remove larger portions of the anterior cornea in a more controlled and often automated manner, which may allow the surgeon to remove more extensive scarring and subsequent irregular astigmatism.8 These techniques, however, depend on the availability and associated cost of corneal allografts.
Excimer Laser
The excimer laser, the use of which lies well within the comfort zone of the refractive surgeon, may hold the key to the future of treating irregular astigmatism and corneal scarring. The FDA first approved excimer laser technology in 1994 for PTK of corneal opacities of the anterior cornea, including scars. PTK, as it is now commonly performed, is limited by its inability to treat irregular astigmatism in a quantifiable manner. With the technique, the surgeon shaves off the elevated portions of the lesion and surrounding cornea. This approach, however, does not actively address the underlying optical issue, although innovative surgeons continue to introduce sophisticated techniques that address this problem. Topography-assisted excimer ablations, ablatable polymers, and wavefront-guided, linked treatments may offer future solutions for patients suffering from irregular astigmatism and corneal scarring.
Several research groups have demonstrated the effectiveness of linking topography devices with excimer lasers to better treat irregular astigmatism. Surgeons may apply Munnerlyn's formula to the measured or derived height of the irregular anterior corneal surface in order to plan tissue ablation at particular points. The Contoured Ablation Pattern (CAP) (VISX, Inc., Santa Clara, CA),9 the OPD-Scan with Final Fit software,10 the Topography Supported Customized Ablations (ToSCA),11 and TopoLink (Nidek, Inc., Fremont, CA)12 have all demonstrated impressive early results in treating irregular astigmatism. At present, topography is not yet linked in real-time to the excimer ablation. Clinicians attempting to improve the smoothness of the treated cornea have suggested using a coupling agent to interact between the laser and the cornea with PTK. Such agents are thought to better transmit the energy of the laser directly onto the cornea and mask. Previously, using the patient's epithelium or varying the viscosity of the artificial tears during PTK has achieved some degree of success in creating a more regular surface on the cornea.5
Frederic K. Kremer, MD, recently reported on the efficacy of a substance called BioMask (Maverick Technologies, Inc. Clearwater, FL), which is a polymer gel that the surgeon molds between the irregular cornea surface and a customized rigid gas permeable contact lens.13 The gel is reported to have the following qualities: an excimer laser ablation rate similar to that of the human cornea; adequate viscosity to fill formal irregularities; excellent adherence to corneal tissue; the ability to be molded to any required curvature; a short solidification time; and easy removal. Results of BioMask in patients with corneal opacities and irregular astigmatism show promise, especially in those with Salzmann's degeneration, those who underwent prior refractive surgery, and/or those who exhibit corneal dystrophies. Patients with previously induced scars did not fair as well in terms of improved BCVA but did show a 50% symptomatic improvement. The authors report that a significant amount of clinical evaluation must be performed with the BioMask. The reported steep learning curve includes canting of the applanator lens and difficulty in handling the polymer.13
Wavefront analysis allows the surgeon to measure any irregularity of the refractive system of the eye and create a template based on the eye's total refractive power. The surgeon then programs an excimer ablation to remove the refractive error, thus producing an aspheric profile with a reduced amount of irregular astigmatism. Theoretically, wavefront-guided ablations will provide a pure refractive-link approach to managing irregular astigmatism. However, another possibility is to create topographic irregularities on the cornea in order to decrease the total aberrations of the visual system. More data are pending for this technique.
CONCLUSION
The problem of corneal scarring with irregular astigmatism is one that vexes the corneal refractive surgeon. In particular, iatrogenic causes from prior surgeries warrant full medical attention. Presently, it appears that there are many treatment avenues we must continue to explore, both with new lamellar keratoplasty techniques and with the excimer laser. Once we understand how to properly combine and apply in real-time corneal topography, wavefront analysis, and ablative polymer masks, we may indeed be able to fully treat these deserving patients.
1. Miller, D, Gurland JE, Isby EK, et al (eds). Human Eye as an Optical System. In: American Academy of Ophthalmology Basic and Clinical Sciences Course. San Francisco: American Academy of Ophthalmology. 1988-1990;108-109.
2. Nordan LT. The Incisional Management of Astigmatism. In: Azar D, ed. Refractive Surgery. Norwalk, Conn: Appleton and Lange. 1997;296-297.
3. Goggin M, Alpins N, Schmid LM. Management of irregular astigmatism. Current Opinion in Ophthalmol. 2000;11:260-266.
4. Eye Bank Association of America. Annual Statistical Report. 1995.
5. Rapuano C. Excimer laser phototherapeutic keratectomy. Current Opinion in Ophthalmol. 2001;12:288-293.
6. Tole DM, McCarty DJ, Couper T, Taylor HR. Comparison of laser in situ keratomileusis and photorefractive keratectomy for the correction of myopia of -6.00 diopters or less. Melbourne Excimer Laser Group. J Refract Surgery. 2001;17:46-54.
7. Alio JL, Artola A, Garcia-Lledo M, et al. Contact lens fitting to correct irregular astigmatism after corneal refractive surgery. J Cataract Refract Surg. 2002;28:1750-1756.
8. Azar DT, Jain S, Sambursky D. A new surgical technique of microkeratome assisted deep lamellar keratoplasty with a hinge flap. Arch Ophthalmol. 2000;118:1112-1115.
9. Tamayo G, Fernandez GE. Early clinical experience using custom excimer laser ablations to treat irregular astigmatism. J Cataract Refract Surg. 2000;26:1442-1450.
10. Gimbel HV, Stoll SB Photorefractive keratectomy with customized segmental ablation to correct irregular astigmatism after laser in situ keratomileusis. J Refract Surg. 2001;17:229-232.
11. Dausch D, Schroder E, Dausch S, et al. Topography controlled excimer laser PRK. J Refract Surg. 2000;16:13-22.
12. Weisinger-Jendritza, Knorz M, Hugger P, et al. Laser in situ keratomileusis assisted by corneal topography. J Cataract Refract Surg. 1998;24:116-174.
13. Kremer F, Aronsky M, Bowyer B, et al. Treatment of corneal surface irregularities using BioMask as an adjunct to excimer laser phototherapeutic keratectomy. Cornea. 2002;21:28-32.