
Cataract surgery has evolved substantially since the traditional procedures of 2 decades ago. The advent of phacoemulsification led this period of dramatic improvements in speed, safety, and precision. In regard to speed and safety, however, there has not been much change. Where significant change has occurred, especially in the past 4 or 5 years, has been in surgeons’ ability to produce superior results. New technology has promoted improved accuracy of uncorrected visual acuity, greater efficiency in running practices and performing procedures, and happier patients. Here are five technologies that have had a significant impact on my practice’s efficiency.
TECHNOLOGY No. 1
Dropless Cataract Surgery
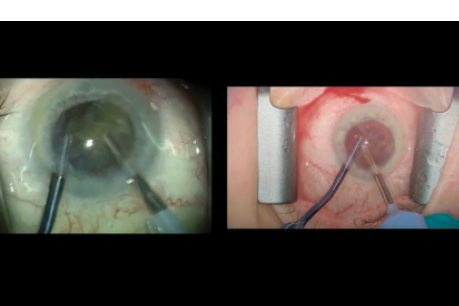
Instead of topical drops, I use a compounded intraocular injection of triamcinolone acetonide and moxifloxacin hydrochloride from Imprimis Pharmaceuticals (Dropless Cataract Surgery) as a transzonular or pars plana injection at the completion of the surgical procedure (Figure 1). Because the need for drops is arguably the most negative aspect of the cataract experience for the patient—and is widely acknowledged to lead to compliance issues—eliminating drops from this process has been invaluable.
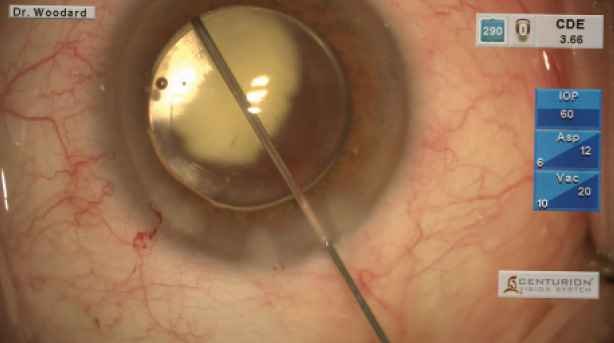
Figure 1. Dropless surgery reduces or eliminates the need for postsurgical drops, compliance concerns, and expenses for patients, while increasing the practice’s efficiency and patients’ convenience.
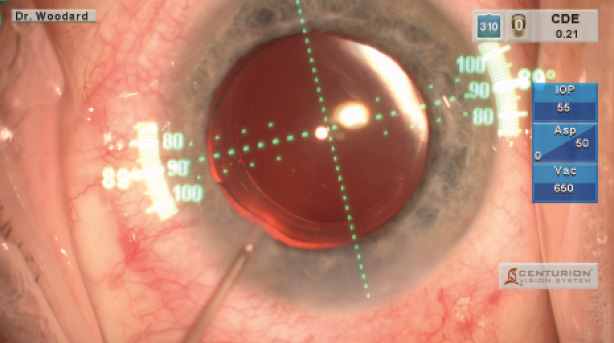
Figure 2. The Verion system indicates correct centration and axial alignment for IOLs.
Implementing dropless surgery has had a much more impressive effect on my practice than I anticipated: it has dramatically minimized the hours my staff spends fielding drop-related phone calls. With administration confusion, cost issues, and patients’ and pharmacists’ inquiries (about substitutions, formulations, cost, etc.), my office was inundated with daily calls. I have a large referral practice, so many patients return to their optometrists for postoperative follow-up, leading to more calls. Dropless therapy has eliminated these issues and minimized chair time.
Watch it Now
Ahad Mahootchi, MD, demonstrates a transzonular technique for placing TriMoxi.
Jonathan Solomon, MD, discusses research that compares toric IOL outcomes using the Zeiss Cataract Suite and the ORA VerifEye+ system.

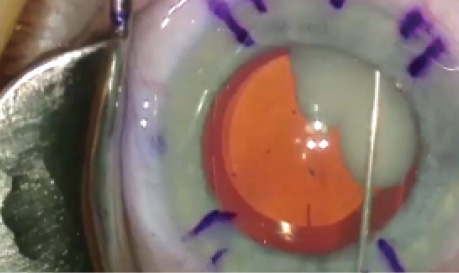
Robert J. Weinstock, MD, presents a split-screen contrast in cataract surgery with and without the use of Omidria.
My clinic has been affected as well. My 1-day postprocedural examinations have shown impressive outcomes. I have found that patients’ eyes are quieter and that their visual acuity is better, resulting in their being happier.
The turnaround time between the initial evaluation and surgery has also decreased notably. In the past, this interval was dictated by the drop regimen; because it was necessary for the patient to begin drops 3 days prior to surgery, a minimum of 4 or 5 days between the evaluation and surgery was unavoidable. Now, there are instances when the evaluation occurs one day and surgery is scheduled for the next. The dropless approach has eliminated waiting, and surprisingly, it has also helped reduce cancellations. I did not realize that patients would often postpone surgery because of concern over the cost of drops.
LISTEN UP
In the opening episode of Ophthalmology off the Grid, Gary Wörtz, MD, invites William Wiley, MD, and Mark Kontos, MD, to dissect the topic of dropless cataract surgery.
My practice has also benefitted from word-of-mouth referrals. Satisfied patients have told their friends. Referring doctors are spreading the word to their colleagues, and many who did not previously refer patients to us are now doing so.
TECHNOLOGY No. 2
ORA With VerifEye+
This wavefront aberrometery system from Alcon has greatly enhanced the accuracy of my results. I value the device’s ability to measure posterior corneal astigmatism and accurately predict the spherical power of the IOL.
In the past, the percentages of my patients who had less than 0.50 D of residual astigmatism postoperatively was not as high as I would have liked. With ORA, my numbers are much improved. When I use this technology, 94% of my toric IOL patients are within ±0.50 D of the intended target postoperatively. I am able to track these data using AnalyzOR Technology incorporated into the system. I also find ORA very helpful in postrefractive surgery patients. In one study of cataract surgery patients who had prior myopic LASIK, 67% were within ±0.50 D of the intended target, and 85% were within ±0.75 D when ORA was used versus 48% and 66%, respectively, with the Haigis L method.1
FROM BMC VISION
READ MORE ON OFFICE EFFICIENCY FROM OUR SISTER TITLES
Postop Cataract Drops on MillennialEye.com
Entering a New World of Cataract Surgery on CRSTodayEurope.com
With fewer of my patients falling outside the intended target, fewer need a LASIK touch-up, IOL exchange, or lens repositioning. Happier patients greatly increase efficiency by reducing postoperative chair time and the need for further procedures.
TECHNOLOGY No. 3
Motorized Optical Tilt Operation
This device by Serj Instruments is installed on my microscope and allows me to tilt the microscope to the desired position with the touch of a button or remote control. I find the technology especially useful when performing microinvasive glaucoma surgery following cataract surgery. The procedure becomes more efficient, because I no longer have to rely on another person in the OR to tilt the microscope. Nor do I need to position the microscope myself. Several predetermined settings can be established, allowing multiple doctors to utilize their own settings. After the procedure, the microscope returns to the original position with the touch of a button or remote control, which helps minimize turnover time between cases. I have found the device reliable, and it has improved the ease and flow of my surgical procedures.
TECHNOLOGY No. 4
Omidria
I use this formulation (phenylephrine and ketorolac injection; Omeros) for my postfemtosecond laser patients. I have found it significantly minimizes the amount of pupillary restriction after laser treatment and is especially helpful in toric lens cases. At times, it is difficult to see the toric markings if the patient’s pupils are not well dilated. My patients’ pupils are significantly more dilated when I use Omidria, and it is similarly useful in my patients who take tamsulosin. I also now need a Malyugin Ring (MicroSurgical Technology) or other instrument for iris manipulation far less often. Omidria has significantly improved my surgical flow and helps me deliver better procedures and outcomes for patients.
TECHNOLOGY No. 5
Verion
Alcon’s image-guided system has been tremendously useful in streamlining my marking process. Composed of a reference unit, a planner, and the digital markers, this system aids in both planning and diagnostics. The unit captures a high-resolution image of the eye, measures keratometry and pupillary size, and detects the anatomical landmarks. In the past, my preference was to perform the markings myself, which required frequent back-and-forth trips during the preoperative process. Verion saves me time and improves my accuracy by reducing the opportunity for human error. I am much more confident about the placement of my incisions and premium lenses (Figure 2).
I have found Verion useful for centering multifocal IOLs as well. The device enables me to center the lens on the preoperative pupil, so patients have better outcomes postoperatively due to improved, consistent centration This benefit was a pleasant surprise.
CONCLUSION
These technologies required a considerable investment, but the clinical and financial returns have been well worth the cost. With these devices, my colleagues and I are able to deliver better outcomes to create happier patients, which in turn increases the practice’s efficiency, growth, and success. n
1. Ianchulev T, Hoffer K, Yoo S, et al. Intraoperative refractive biometry for predicting intraocular lens power calculation after prior myopic refractive surgery. Ophthalmology.2014;121(1):57-60.




