

Gelatinous drop-like corneal dystrophy (GDLD) is predominantly found in people of Japanese descent. This autosomal recessive disorder typically manifests as a jelly-like form on the cornea, results in severely impaired visual acuity (VA), and likely requires corneal transplantation. Most often, the disorder appears in the first decade of life and is bilateral.
We report on a consanguineous Mexican family affected in two generations by GDLD. We subsequently performed three simultaneous corneal transplants on the family at Instituto de Oftalmología “Conde de Valenciana” in Mexico City, courtesy of corneal tissue donation from the Foundation of the Lions Eye Institute for Transplant and Research (LEITR).
THE FAMILY
We heard about the first patient when she presented to us because she had undergone penetrating keratoplasty in her right eye that was now failing 2 years postoperatively. Adelina was 35 years old at the time and had a VA of light perception in both eyes. Her main complaints (aside from failing vision) were photophobia and foreign body sensation. We performed a differential diagnosis on her to exclude other corneal dystrophies, but we were confident based on her physical presentation—white-yellowish nodular opacities on the visual axis and anterior stromal neovascularization—that it was GDLD. Meanwhile, her left eye showed vascularization and stromal amyloid deposits with yellowish-white nodular lesions in a mulberry pattern and opacity involving the visual axis.

Figure 1. Preoperatively, the female sibling had obvious signs of GDLD, including the mulberry-like pattern opacities. (Note: all images are of the two siblings and not the first family members identified with GDLD.)
Once we confirmed our suspicions of corneal dystrophy, Adelina told us she had siblings and a son who suffered the same symptoms. This family lives in a remote region of the Oaxaca region in the Mexican mountains and do not speak Spanish (they speak an indigenous language). Adelina’s community is very poor, so we traveled to her village to determine if we could restore some sight and help improve their lives. We convinced her family to come to our facility (at our cost) to be tested and treated.
Adelina’s brother was 21 years old, presenting with poor vision, photophobia, and longstanding foreign body sensation. His VA was 20/200 OU. Adelina’s sister was 19 years old, with a VA of 20/100 OD and 5/200 OS. On slit-lamp examination, both siblings had the same clinical findings as Adelina. (Figure 1 is Adelina’s female sibling, and Figure 2 is Adelina’s male sibling.) Adelina’s son was 14 years old and had a VA of 20/30 OD and 20/40 OS. On slit-lamp examination, both eyes showed incipient yellowish-white lesions, but the visual axis was involved in the right eye only. We found a novel TACSTD2 gene mutation after performing a genomic analysis for all affected family members in the genetics department at our facility.
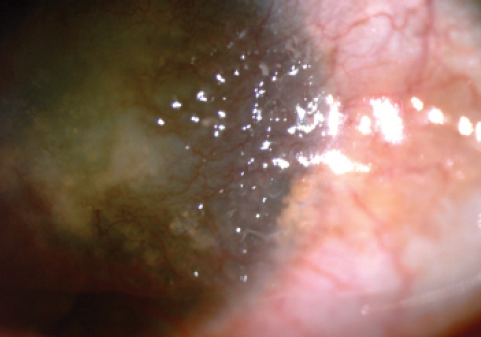
Figure 2. The male sibling also had obvious signs of GDLD, including the yellowish nodular lesions.

Figure 3. In postoperative month 3, the graft remains clear on the female sibling.
THE LOGISTICS
After confirming the diagnosis, the logistics of coordinating transportation to our facility meant we wanted to perform simultaneous surgeries On the three family members who were eligible. Our facility serves the entire country as the main site for corneal repair, but it is located 10 hours from Adelina’s village.
We contacted LEITR to request donor corneas, as it is rare for us to have three available corneas at one time. LEITR also performs background screenings on all of its donor tissue via slit lamp (to confirm corneal health) and specular microscope (to ensure an adequate number of cells). For these surgeries, we needed three corneas to be roughly the same death-to-preservation time, and the corneas we had at our facility did not meet our criteria for this family.
SURGICAL OUTCOMES AND PLANNED FOLLOW-UP
Graft survival is usually reduced in GDLD. Our results to date are short term, but 3 months after surgery, all corneal grafts were transparent. We are hoping to avoid graft failure by being somewhat vigilant and scheduling follow-up visits every few months.
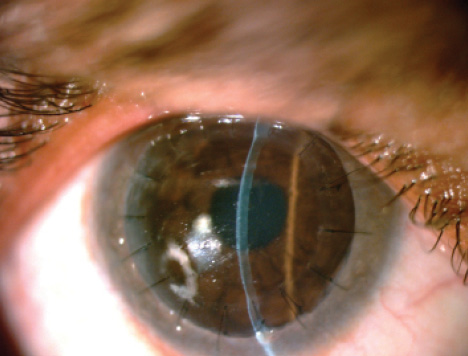
Figure 4. Postoperatively at the slit lamp, the male sibling’s graft looks clear.
So far, everyone in Adelina’s family is doing well; they are able to contribute to their village again with housework and working in the fields. They are able to get on a bus to our facility on their own. The improvement in their quality of life has been outstanding (Figure 3 is Adelina’s sister postoperatively, and Figure 4 is Adelina’s brother after surgery.)
In short, LEITR’s corneas and our surgical expertise resulted in a family’s being able to participate fully in society again, be relatively autonomous again, and be a productive part of their community. n
Enrique O. Graue -Hernández, MD, MSc
• chief of the Cornea & Refractive Surgery Department, Instituto de Oftalmología Conde de Valenciana, Universidad Nacional Autónoma de México, Mexico
• +521 554 369 1300; egraueh@gmail.com
Jesus Cabral-Macias, MD
• fellow of the Cornea and Refractive Surgery Department, Instituto de Oftalmología Conde de Valenciana, Universidad Nacional Autónoma de México, Mexico
• +521 554 369 1300; jcabralmacias@hotmail.com


