Tecnis Toric IOL
BY DANIEL H. CHANG, MD

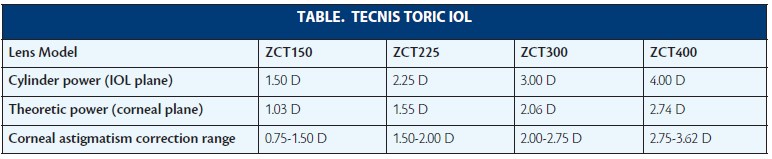
Since its FDA approval in 2013, I have found the Tecnis Toric IOL (model ZCTXXX; Abbott Medical Optics [AMO]) to be an exceptional lens for helping patients who desire correction of their astigmatism at the time of cataract surgery (see Table). Built on the basic platform of the Tecnis 1-piece IOL (AMO), the toric lens has all of the advantages inherent in the platform with the addition of excellent astigmatic correction.
OPTICS
In terms of optics, the Tecnis Toric IOL (Figure) is made of a midindex acrylic material (refractive index of 1.47) that has the highest published Abbe Number (55) of any foldable IOL and thus the lowest chromatic aberration of any toric IOL available in the United States.1,2 The implant provides -0.27 µm of spherical aberration, which fully corrects the average cornea, producing a sharper quality of vision and contrast sensitivity than spherical lenses.3 In my experience, the lens combines effective chromatic aberration properties with the correction of spherical aberration to offer excellent functional vision and vision in dim light.
Another advantage of sharing the same platform as the Tecnis 1-piece family of IOLs is that the toric model uses the same Unfolder Platinum 1 Series implantation system (AMO), which I have found to provide consistent injection and unfolding. In my hands, rotating and positioning the lens is easy and precise, with fine adjustments in both the clockwise and counterclockwise directions possible. Once the lens is in place, the posterior vaulting of the optic relative to the haptics has some forgiveness with respect to the anterior capsulotomy’s size, shape, and position, and it also helps to maximize contact of the optic with the posterior capsule to prevent the entrapment of viscoelastic and augment stability.

Figure. Tecnis Toric IOL.
EXCELLENT OUTCOMES
In my experience, these design features contribute to excellent visual and refractive outcomes as well as superb rotational stability. The Tecnis Toric IOL easily meets the American National Standards Institute’s Z80.30-2010 standards for toric IOL rotational stability. In the FDA premarket approval study, between 1 and 3 months, 93% of eyes showed less than 5º of rotation, and between 3 and 6 months, 94% of eyes demonstrated less than 5º of rotation. The average rotation between baseline and 6 months was 2.74º.3 Of the nearly 200 Tecnis Toric IOLs that I have implanted to date, I have only had to return to the OR to rotate one.
CONCLUSION
Superb optics and excellent rotational stability translate into great outcomes. In the FDA premarket approval study, 94% of patients implanted with the ZCT150 lens achieved less than or equal to 1.00 D of residual astigmatism, and 72% of patients achieved less than or equal to 0.50 D of residual astigmatism. This meant that 89% of patients with the Tecnis Toric ZCT150 achieved 20/32 or better distance UCVA.
1. Zhao H, Mainster MA. The effect of chromatic dispersion on pseudophakic optical performance. Br J Ophthalmol. 2007;91:1225-1229.
2. Negishi K, Ohnuma K, Hirayama N, Noda T. Effect of chromatic aberration on contrast sensitivity in pseudophakic eyes. Arch Ophthalmol. 2001;119:1154-1158.
3. Tecnis 1-Piece IOL [package insert]. Abbott Park, IL: Abbott Medical Optics; 2013.
Trulign Toric
By Jay Pepose, MD, PhD

Introduced in 2013, the Trulign Toric IOL (Bausch + Lomb) is a toric version of the company’s Crystalens AO. The former features a toric optic on the posterior surface and two axial orientation markings on the anterior surface. Its design (5-mm biconvex optic made of a fourth-generation silicone, two hinged-plate haptics, and four polyimide loops) is otherwise the same as the AO model. The Trulign Toric lens is intended for primary implantation in the capsular bag of the eye for the visual correction of aphakia and postoperative refractive astigmatism secondary to removal of a cataractous lens in adult patients with or without presbyopia who desire a reduction of residual refractive cylinder, increased spectacle independence, and improved near, intermediate, and distance UCVA.
ADDRESSING UNMET NEEDS
The Trulign Toric (Figure) is the first lens to address two important previously unmet clinical needs of cataract patients in a single procedure. The first is offsetting substantial preexisting corneal astigmatism, which has an impact on more than one in three patients. The other is patients’ desire to have excellent uncorrected distance and intermediate vision with improved near vision. Standard toric IOLs correct astigmatism but improve visual acuity only at a single distance. Therefore, many patients who receive these lenses still rely on glasses for everyday activities such as using a computer. In my experience, Trulign Toric and Crystalens AO patients have exceptional intermediate and distance vision and are much more independent of glasses than standard monofocal patients. I also find that the former have less dysphotopsia at night than many patients with multifocal IOLs. People who use computers and tablets and those who play golf, tennis, and other sports are great candidates for these lenses. I advise patients that they may, depending on the print size and illumination, need glasses to read, but otherwise, they are mostly spectacle independent. In some patients, I offset the nondominant eye to create mini-monovision, which further enhances their depth of field.
As medical monitor for the Trulign IOL’s clinical trial, I am intimately familiar with its unique features and exceptional performance. The results of the trial showed that the implant was safe and effective in reducing the effects of preoperative corneal astigmatism and that it provided excellent uncorrected distance and intermediate vision and functional near vision.1 The study also indicated that the Trulign was about equally effective in reducing refractive cylinder regardless of the degree of preexisting corneal astigmatism, with no new safety concerns or an increase in visual disturbances associated with the toric modification to this IOL platform.1
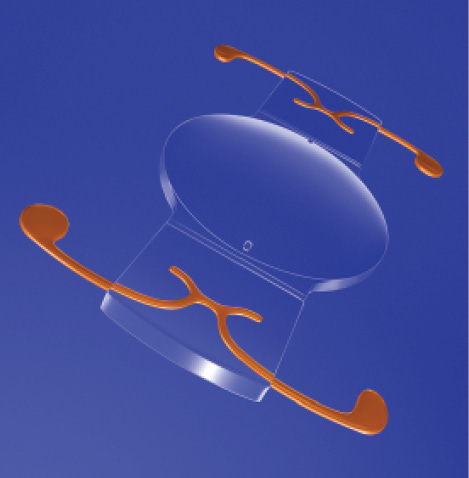
Figure. Trulign Toric IOL.
ROTATIONAL STABILITY
Also noteworthy is this IOL’s rotational stability, which may in part be due to the polyimide loops (Figure). This is a key feature, as each degree of off-axis rotation results in a 3.3% loss of the toric effect.1 Most toric lenses can be rotated in only one direction. Because of the Trulign Toric’s uniform design, I can rotate the lens either way, without worrying about overrotation. In the clinical trial, the unique haptic design provided excellent rotational stability, with 96.1% of the lenses rotating less than 5º from the day of surgery to 4 to 6 months postoperatively.1
The Trulign is now available in powers ranging from 10.00 to 33.00 D in cylinders of 1.25, 2.00, and 2.75 D.
CONCLUSION
I value this lens for its ability to treat cataract and corneal astigmatism in one procedure, its ability to provide excellent uncorrected distance and intermediate vision, and its exceptional performance and safety.
1. Pepose JS, Hayashida J, Hovanesian J, et al. Safety and effectiveness of a new toric presbyopia-correcting posterior chamber silicone intraocular lens. J Cataract Refract Surg. 2015;41:295-305.
STAAR Toric
By Thomas M. Harvey, MD

Easily one of the most underutilized toric implants in the world, the STAAR Toric IOL (STAAR Surgical) has several unique features that are worth highlighting. Among them, it has the longest track record—more than 15 years—of any toric implant in the United States. It is the only single-piece silicone toric IOL available in this country. The spherical optic is not subject to the long-term formation of water microvacuoles (glistenings), and it has a low refractive index (1.413). The implant’s plate-haptic configuration allows positioning in a clockwise or counterclockwise fashion. It has only two cylinder powers, which usually makes a toric calculator unnecessary.
The results of modern cataract surgery far outshine those of the original procedure. How has that been accomplished? Technological (eg, advanced biometry, calculations) and technical (eg, complete cortical and lens epithelial cell evacuation) advances have made outcomes more predictable. A new emphasis on the capsulotomy’s size and uniformity as well as a greater understanding of capsular bag dimensions may also bear fruit.
The STAAR Toric IOL’s optical biometry A-constant is 118.5. The 2.00 D version corrects (on average) 1.50 D at the corneal plane. The +3.50 D version corrects (on average) 2.25 D at the corneal plane. A 5.5-mm capsulorhexis is ideal for this IOL, and thorough removal of cortical material as well as lens epithelial cells is beneficial. A cohesive ophthalmic viscosurgical device (OVD) should completely fill the capsular bag prior to the IOL’s insertion.
TIPS FOR SUCCESS WITH THIS LENS
A 2.75-mm incision is recommended for the STAAR Toric IOL’s insertion with the syringe-style injection system. Wound-assist with the MSI cartridge tip just inside the anterior chamber is reproducible and safe, in my experience. The IOL opens rapidly, so I recommend not having the cartridge tip too far into the anterior chamber. Surgeons who use intraoperative aberrometry enjoy the rapid opening to avoid unnecessary unfolding delay.
A “test-positioning step” before OVD removal is advantageous to align the IOL on its intended axis. If the dimensions of the capsular bag are large, the IOL will rotate too easily, which necessitates use of a capsular tension ring (eg, EyeJet with Morcher 14C; FCI Ophthalmics) to achieve rotational stability. Finally, complete removal of the OVD under and around the IOL is suggested.
Why should one consider a nonaspheric optic? Most cataract patients have small pupils. Asphericity has been shown to be of benefit when there is a large low-mesopic pupil; a pupil at or below 4 mm may not require spherical aberration correction.1 Even young patients have (under dim conditions) a 6.5-mm or smaller pupil on average.2 This size is not commonly encountered in most cataract clinics. Moreover, aspheric optics could degrade the visual acuity and contrast sensitivity of many patients with a history of hyperopic laser vision correction and others with virgin hyperprolate corneas. It has also been recognized that a spherical optic may provide a greater depth of focus than an aspheric optic.3
ROTATIONal STABILITY
When new technology came to market, the knock against the STAAR Toric IOL was relative rotational instability. The lens was rumored to spin within the capsular bag. Much has changed. The implant is now longer for most powers (11.2 vs 10.8 mm). It has larger apertures that allow fibronectin adhesion between anterior and posterior capsular leaflets. The micro-etched haptic may resist slipping when against the capsule. Complete cortical and lens epithelial cell removal minimizes the risk of late asymmetric capsular fibrosis. Importantly, if one side zippers closed, it can actually cause the lens to rotate later. Repositioning rates of 1.5% (with 90% of IOLs ≤ 10º misalignment) can be expected using the longer platform.4
CONCLUSION
The STAAR Toric IOL is a useful option to avoid Z syndrome, material decomposition, unwanted Purkinje reflexes, and dysphotopsias. In my hands, this lens works well in small eyes, especially those that have undergone hyperopic keratorefractive surgery. Patients with excessive “pathologic” asphericity (eg, subclinical keratoconus) can also benefit greatly from this technology by simultaneously correcting astigmatism while avoiding excessive asphericity induction.
1. Calossi A. Corneal asphericity and spherical aberration. J Refract Surg. 2007: 505-514
2. Ho LY, Harvey TM, Scherer J, et al. Comparison of Rosenbaum pupillometry card using red and blue light to Colvard and Iowa pupillometers. J Refract Surg. 2009:1-7.
3. Nanavaty M, Spalton DJ, Gala KB. Fellow-eye comparison of 2 aspheric microincision intraocular lenses and effect of asphericity on visual performance. J Cataract Refract Surg. 2012: 625-632.
4. Chang DF. Comparative rotational stability of single-piece open-loop acrylic and plate-haptic silicone toric intraocular lenses. J Refract Surg. 2008:1842-1847.
AcrySof Toric IOL
BY DAMIEN GOLDBERG, MD

A large percentage of the people presenting for cataract surgery have visually significant astigmatism. A recent 6,000-eye analysis of corneal cylinder by Warren Hill, MD, concluded that more than 52% of patients had 0.75 D of astigmatism or more.1 When managing astigmatism, I always try to achieve less than 0.25 D of residual astigmatism and to get as close to zero as possible. Studies have shown that as little as 0.50 D of astigmatism can reduce visual acuity by 1 line and that it will have an even greater impact in the real world in low-contrast situations like driving or reading at night.2
When it comes to surgically managing astigmatism, I have the greatest confidence using the AcrySof Toric IOL (Alcon). This lens now has a 10-year track record. During the FDA trial of the AcrySof IQ Toric IOL, 97% of patients who received the lens bilaterally were spectacle free for distance vision.3 Moreover, owing to its bioadhesion characteristics, the AcrySof IQ Toric lens exhibits minimal rotation (< 5º) at 6 months.3
Although cataract surgery has become more sophisticated with the use of image-guided systems and intraoperative aberrometry, I would argue that beginning and established surgeons alike can easily improve patients’ visual outcomes by adopting AcrySof Toric IOL technology. When the lens’ trial data were released in 2005, many patients enrolled had their eyes marked with ink pens, and all keratometry readings were determined manually. Despite these basic measurements, the majority of the patients achieved spectacle freedom for distance vision.3 With today’s technology, results with these toric IOLs will be even better, and the range of correction offered by this lens is wide (Figure 1).
EDUCATIONAL RESOURCE
To improve outcomes and techniques, I recommend consulting the Toric Pro app, Alcon’s multimedia educational tool (Figure 2). Designed for the iPad (Apple), this app can be downloaded for free through the Apple iTunes store. It will soon be available on PC as well and can be viewed using Adobe Air16. The app provides references and resources to help surgeons of all levels become more comfortable with implanting toric lenses. Several sections within the app, including a program that allows surgeons to better predict their surgically induced astigmatism (Figure 3), allow ophthalmologists to fine-tune their surgical outcomes. There are some instructive videos that users can watch to hear experts like Bonnie An Henderson, MD, and Stephen Scoper, MD, discuss counseling patients and improving surgical techniques (Figure 4).

Figure 1. The AcrySof Toric IOLs have a wide range of cylinder powers.

Figure 2. The Toric Pro app is a multimedia tool now available for the iPad.
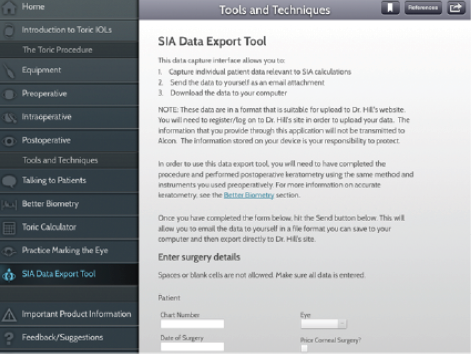
Figure 3. The nomogram on the Toric Pro app can help surgeons determine their surgically induced astigmatism.

Figure 4. Watch Bonnie An Henderson, MD, on the Toric Pro app perform surgery using the Acrysof Toric IOL.
CANDIDATES
Potential candidates for toric lenses should have regular astigmatism and desire glasses-free distance vision. Experienced surgeons may choose to use the technology for some patients with irregular astigmatism, but this should only be done on a case-by-case bases.
TIPS FOR SUCCESS
To determine the correct toric IOL power, I still use the Alcon Toric Calculator, but another option is the new Barrett Toric Calculator (www.ascrs.org/barrett-toric-calculator). When preparing for surgery, I strongly recommend accounting for surgically induced astigmatism as well as the placement of the primary corneal incision. It does not matter where the surgeon chooses to operate, as long as he or she feels comfortable and the biometery adds up.
Recent data suggest that posterior curvature may affect the refractive outcome.4 To take that into consideration, when I operate on eyes that have with-the-rule astigmatism, I subtract 0.30 D from my toric diopter correction. For against-the-rule astigmatism, I add 0.30 D.
Cataract surgery with toric IOLs is not a great leap from standard cataract surgery, and I recommend all surgeons explore adopting this technology. n
1. Hill W. IOL power calculations: how to achieve accurate results. http://www.doctor-hill.com/iol-main/iol_main.htm. Accesssed May 19, 2015.
2. Lane SS, Ernest P, Miller KM, et al. Comparison of clinical and patient reported outcomes with bilateral AcrySof Toric or spherical control intraocular lenses. J Refract Surg. 2009;25:899-901.
3. Watanabe K, Negishi K, Kawai M, et al. Effect of experimentally induced astigmatism on functional, conventional, and low-contrast visual acuity. J Refract Surg. 2013;29(1):19-24.
4. Koch DD, Ali SF, Weikert MP, et al. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38:2080-2087.
Daniel H. Chang, MD
• partner at Empire Eye and Laser Center in Bakersfield, California
• (661) 325-3937; dchang@empireeyeandlaser.com
• financial disclosure: consultant to Abbott Medical Optics
Jay S. Pepose, MD, PhD
• founder and director of the Pepose Vision Institute, Chesterfield, Missouri
• professor of clinical ophthalmology and visual sciences at the Washington University School of Medicine in St. Louis
• (636) 728-0111; jpepose@peposevision.com
• financial disclosure: consultant to Abbott Medical Optics and Bausch + Lomb, medical monitor for the Trulign Toric IOL clinical trial
Thomas M. Harvey, MD
• Chippewa Valley Eye Clinic, Chippewa Falls, Wisconsin
• tharvey@cv-eye.com
• financial disclosure: consultant to STAAR Surgical
Damien Goldberg, MD
• private practice at Wolstan & Goldberg Eye Associates, Torrance, California
• (310) 543-2611; goldbed@hotmail.com; Twitter @damiengoldberg1
• financial disclosure: consultant to Alcon