Case Presentation

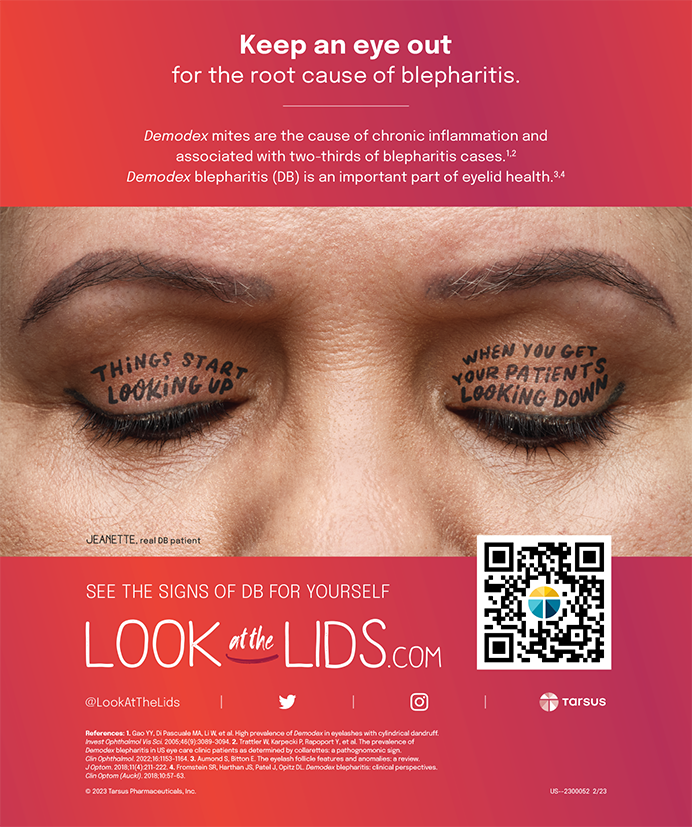
Figure 1. Appearance of the patient's post-RK right eye at the slit lamp.

Figure 2. Topography (Tomey) of the patient's right eye after RK.
CRAIG BEYER, DO
The key features I review when deciding upon a treatment plan are
• age
• previous surgery
• corneal curvature and thickness
• degree of refraction
• lenticular status
• BSCVA
• occupation and hobbies
I then choose one of the five refractive procedures my practice offers: PRK, LASIK, corneal collagen cross-linking (not FDA approved), the Visian ICL (STAAR Surgical), and refractive lens exchange (RLE).
At the 2014 annual meeting of the American Society of Cataract and Refractive Surgery, Kent Stiverson, MD, and others presented data on the successful performance of more than 18,000 cataract surgeries in the minor procedure room of the Kaiser Foundation, located in Lafayette, Colorado.1 Kaiser continues to perform hundreds of these procedures per month and, unquestionably, has established a new standard of care in Boulder County for IOL surgery. As of April 2015, my practice also began successfully performing RLE, cataract surgery, and implantation of the Visian ICL in its minor procedure room under a class “A” surgical protocol.
RK patients do very well with PRK using adjunctive mitomycin C because their corneal curvature is flat, allowing for sufficient central steepening after PRK. Visual recovery after PRK over RK typically takes longer than PRK on virgin corneas, because the RK incisions cause surface irregularity after PRK. In my experience, however, reapplying a bandage contact lens (Acuvue Oasys with an 8.8-mm base curve; Vistakon) 1 week after PRK and leaving it in place for up to 2 weeks help the epithelium thicken between incisions and thus speed up the recovery process.
Because of this patient's age, presbyopia, early nuclear sclerosis, and desire for near vision, my first choice would be RLE with a Crystalens (Bausch + Lomb) in his right eye, as long as the pupillary size is suitable. Postoperative recovery will be much faster than with PRK, and once the patient recognized substantial improvement in the distance and near vision in his right eye, I expect he would elect the same procedure for his left eye.
PREEYA K. GUPTA, MD
Like many patients who have undergone RK for the correction of myopia, this patient is experiencing progressive consecutive hyperopia in his right eye. He is myopic in his left eye and now presbyopic in both eyes. Important factors are the early cataract formation and his age.
My first steps in approaching vision correction in a post-RK eye are to assess the topography and examine the radial incisions for gaping. The topography in this case is consistent with irregular astigmatism after RK, but the patient's visual acuity corrects to 20/20 OU. It would be important to assess his BCVA; in cases in which patients received an excessive number of radial incisions, the topography can be very irregular, and the resultant irregular astigmatism can only be treated with a hard contact lens.
I would present the patient with two options:
1. RLE in the left eye with a low-add Tecnis Multifocal IOL (ZKBOO; Abbott Medical Optics) or a monofocal IOL targeted for distance and RLE in the right eye using a monofocal IOL with a target of -0.75 or -1.00 D
2. LASIK on the left eye aimed for plano and PRK on the right eye with a near target (about -1.00 to -1.50 D of myopia)
No matter which option the patient chooses, he must understand that a post-RK cornea can continue to change over time. Given the early cataracts and his age, I would prefer option 1. This approach will provide a better long-term solution than option 2, because the cataract will no longer lead to progressive refractive changes. I would avoid a multifocal IOL in the patient's right eye for two reasons. First, I would expect gradual worsening of the hyperopia. Second, higher-order aberrations induced by the RK incisions might degrade the vision quality achieved with a multifocal lens. I would expect targeting some myopia in the right eye to make the progressive hyperopia less of a problem over time. The multifocal IOL in the patient's left eye should provide him with excellent distance and near vision over the years. It would be important to explain to him that there is variability in post-RK biometry and that an enhancement with laser vision correction may therefore be needed.
ROBERT K. MALONEY, MD
Nuclear sclerosis in a post-RK eye is a contraindication to laser refractive surgery, because the cataract can cause a decrease in vision disproportionate to the degree of nuclear sclerosis. This presumably occurs because the aberrations induced by the RK procedure accentuate the aberrations induced by the early cataract. In the setting of nuclear sclerosis, RLE would certainly be the procedure of choice for this patient's right eye.
Unfortunately, RLE after RK is relatively inaccurate, even more so than cataract surgery after LASIK, which is less accurate than in an eye with no history of refractive surgery. For this reason, RLE in patients after RK should be approached cautiously. In my experience, however, many doctors who call “trace” nuclear sclerosis in a 54-year-old are merely referring to the normal lenticular changes that occur with age. Such changes are not a contraindication to laser refractive surgery and are consistent with excellent postoperative visual acuity.
For that reason, after examining the patient myself, I would probably recommend laser refractive surgery. If the incisions are well healed without epithelial plugs, as they are here, I favor LASIK with a microkeratome. If there are epithelial plugs, PRK with mitomycin C is my preferred approach. One could consider LASIK with a femtosecond laser flap, but lifting the flap could lead to separation of the RK incisions, increasing the risk of epithelial ingrowth.
My analysis of the left eye is similar. The sharp 20/20 visual acuity implies that the nuclear sclerosis is insignificant. If the trace nuclear sclerosis is merely consistent with the patient's age, either LASIK or a Visian ICL could be considered. The latter will provide better night vision. In the presence of even mild true nuclear sclerosis, RLE would be my procedure of choice. One should certainly consider a monovision correction in the patient's left eye to reduce his dependence on reading glasses. n
1. Stiverson K, Kloor J, Litoff D. Bilateral cataract surgery in the Colorado Permanente Medical Group. Presented at: 2014 ASCRS/ASOA Congress & Symposium; April 27, 2014; Boston, MA.
Section Editor Alan N. Carlson, MD
• professor of ophthalmology and chief, corneal and refractive
surgery, Duke University Eye Center, Durham, North Carolina
Section Editor Stephen Coleman, MD
• director of Coleman Vision, Albuquerque, New Mexico
• (505) 821-8880; stephen@colemanvision.com
Section Editor Karl G. Stonecipher, MD
• director of refractive surgery, TLC in Greensboro, North Carolina
Craig Beyer, DO
• medical director, Beyer Laser Center, Boulder, Colorado
• (303) 499-2020; cbeyer@bouldereyes.com
• Financial disclosure: None acknowledged
Preeya K. Gupta, MD
• assistant professor of ophthalmology, Duke Eye Center, Durham,
North Carolina
• (919) 660-5071; preeya.gupta@duke.edu
• financial disclosure: consultant to Abbott Medical Optics
Robert K. Maloney, MD
• director, Maloney Vision Institute, Los Angeles
• (310) 208-3937; info@maloneyvision.com
• Financial disclosure: None acknowledged