Learning to perform cataract surgery is one of the most important components of new ophthalmologists’ training. Residents must serve as the primary surgeon on at least 86 cataract procedures— far more than for any other single procedure and accounting for about half of the total surgical requirement during residency.
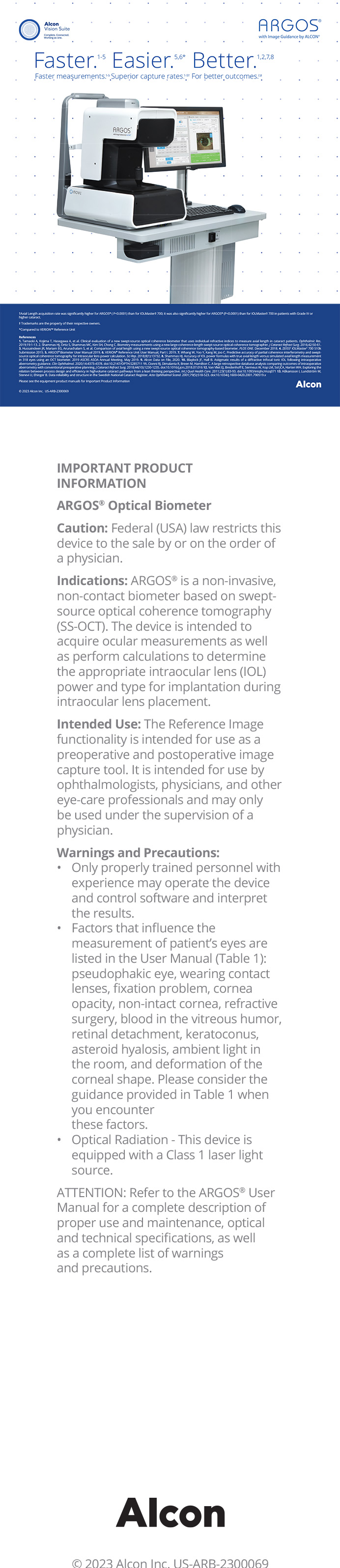
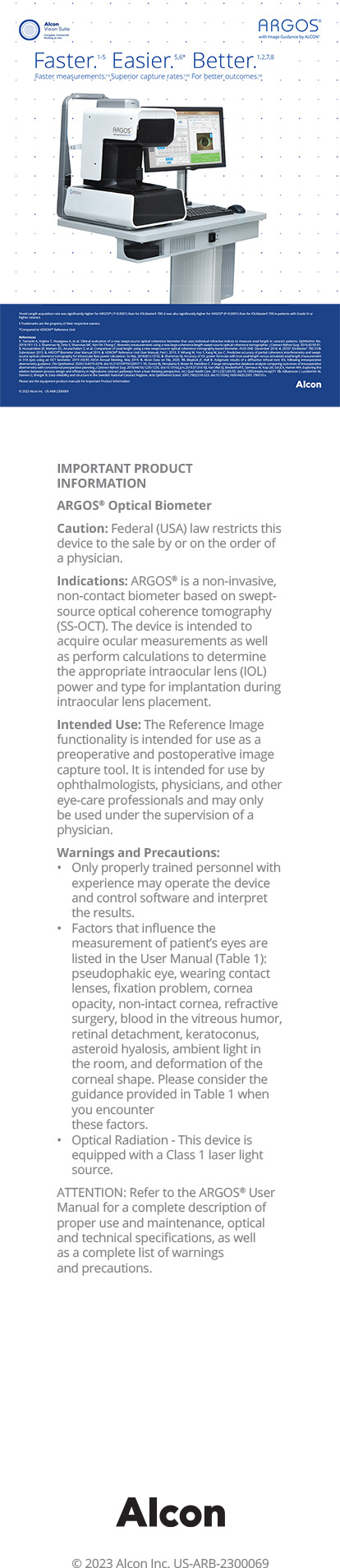
At Wills Eye Institute in Philadelphia, we have long believed that residents should learn all of the latest cataract techniques, and we ensure that they have access to the same technologies that we attending surgeons use in our private practices. This is somewhat unusual. The Young Physicians & Residents Committee of the American Society of Cataract and Refractive Surgery (ASCRS) recently reported that residents, fellows, and young ophthalmologists, on average, have very limited exposure to advanced elective technologies such as excimer and femtosecond lasers and premium IOLs (Figure 1).1
Wills’ residents are given extensive exposure to toric and multifocal IOLs, and ours was one of the first residency programs in the United States to have access to a laser cataract platform (Figure 2). This year, 100% of our graduating residents will leave the program already certified to perform laser cataract surgery with the Catalys Precision Laser System (Abbott Medical Optics). Initially, the manufacturer provided technicians to supervise residents’ laser training toward certification. Now, we have three attending surgeons who are qualified to proctor certification training, which makes giving residents access even easier.
DEBUNKING MYTHS
Premium Technologies Will “Take Over”
Some might argue that residents should not have access to a femtosecond laser before they have mastered manual cataract surgery, but we have found that the two methods can be taught in tandem. In any residency program, laser cataract cases are likely to represent a small proportion of total cataract surgery volume. At Wills, for example, residents perform significantly more than the required minimum number of surgical cases. Out of an average of 175 cataract procedures during residency, perhaps 10 to 12 will involve the laser. Residents still have plenty of opportunity to become proficient at standard phaco and manual techniques, as they should.
In the near term, I do not anticipate that any of the premium technologies we use will take over as the default approach that residents learn. Although our industry partners have been generous in providing complimentary multifocal and toric IOLs and femtosecond laser patient interfaces for use in resident education, there is a natural ceiling on the penetration level of these technologies among residents.
Nobody Will Want to Have Premium Surgery Performed by a Resident
It is probably true that patients paying full price out of pocket for laser cataract surgery and a multifocal IOL will want a more experienced surgeon. Manufacturers’ provision of free interfaces and IOLs for residents, however, opens up the opportunity for some patients to have the benefits of a multifocal IOL or a laser procedure at no additional charge.
At the Storm Eye Institute of the Medical University of South Carolina in Charleston, residents also have access to a femtosecond laser. Surgeons there recently reported that laser cataract procedures were just as safe as standard phacoemulsification in the hands of residents. 2. Not surprisingly, cumulative energy dissipation in the laser cases was about half that in the standard phaco cases. There was also a trend toward fewer complications and less endothelial cell loss in the laser cases.
The opportunity to use a laser may make it safer for residents to perform surgery in certain cases. We let them select the cases in which they will use the laser, and I have been intrigued to see how different their choices are from my own. In most private practice and university settings, where use of the laser is limited to patients who are paying for a refractive procedure, surgeons typically offer it only for the treatment of relatively uncomplicated eyes with 20/20 visual potential. Many surgeons offer premium procedures disproportionately to patients at the younger end of the spectrum who they believe may have more to gain from (or more years to enjoy) their refractive correction. In contrast, our residents choose to use the laser for older, more medically challenging cases, such as patients with pseudoexfoliation or Fuchs dystrophy, where reduced ultrasound energy and a perfect capsulotomy are highly beneficial and a resident’s lack of experience can be most problematic. Experienced surgeons may learn some important lessons from residents’ experiences with the laser cataract procedure in these eyes.
Residents’ Access to the Laser Will Pose a Scheduling Burden
Our OR coordinators were convinced that adding the laser would slow down the whole schedule for resident cases. At Wills, the laser and the phaco machine are in the same OR. Although the laser offering adds an extra surgical step, its use has facilitated and expedited the phaco portion of the cataract procedure so that total OR time for a resident is the same or perhaps slightly less.
ADVANTAGES
There are several reasons to make training residents to perform laser cataract surgery a priority. Patients in our residents’ clinic have been thrilled to have access to the latest procedures. The technology we offer augments their morale and makes the institution attractive to future students and residents.
Moreover, I believe that exposing residents to everything that is available in ophthalmology greatly benefits their development as young surgeons. According to the ASCRS 2013 Clinical Trends Survey, use of a femtosecond laser is expected to increase from less than 10% of cases in 2013 to nearly 30% within 5 years (Figure 3). Hands-on experience with new technology early in their careers makes its adoption easier once residents are in practice. Certification and experience with premium technologies before they enter practice are an asset on their résumés: they say a great deal about the depth and breadth of residents’ training and the skill set they bring to a practice.
Mark H. Blecher, MD, is codirector of the Cataract Service at Wills Eye Institute in Philadelphia, and he is in practice at Philadelphia Eye Associates. He is a paid consultant to Abbott Medical Optics. Dr. Blecher may be reached at (215) 339-8100; mhbmd@comcast.net.
- Yeu E, Reeves SW, Wang L, Randleman JB. 2013 survey of the ASCRS Young Physicians & Residents Committee. J Cataract Refract Surg. 2013;39:279-284.
- Femtosecond laser-assisted cataract surgery found safe for resident training. Ocular Surgery News. May 30, 2014. http://www.healio.com/ophthalmology/cataract-surgery/news/online/%7B7dccb6af-230d-4bca-a69d- 4ba9769b0a8f%7D/femtosecond-laser-assisted-cataract-surgery-found-safe-for-resident-training. Accessed August 11, 2014.