When I was a first-year resident, I had a chief who amazed me. This was not because of his surgical skills or his intelligence, but because of his ability to walk into a busy clinic, stand next to me, and guess the diagnosis of each patient in the waiting room without examining him or her. Based on the patients’ composure and the general appearance of their eyes, amazingly, he was often right, but not always. He often missed the dry eye patients.
What does a patient with dry eye disease (DED) look like? Once we resist the temptation to imagine our favorite DED patient, the one who haunts our dreams at night, we have to admit to ourselves that imagining the typical patient with DED is not easy. Both the disease and the person who bears the disease are remarkably diverse; some patients cannot be convinced they have a disease worth treating, while others are consumed by the diagnosis. The pathophysiologic variability that characterizes aqueous-deficient and evaporative DED pales in comparison to the variability that characterizes patients’ perceptions of DED.
LESSONS FROM PSYCHIATRY
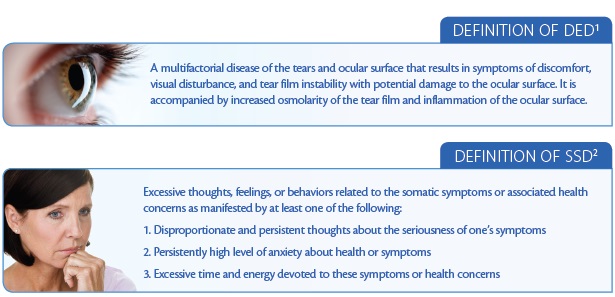
Although we undoubtedly have become familiar with the Dry Eye Workshop (DEWS) definition of DED (see Definition of DED),1 most ophthalmologists are not acquainted with the definition of somatic symptom disorder (SSD; see Definition of SSD) in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).2 Patients with this diagnosis tend to channel significant anxiety into their disease state.
These are the patients who require excessive chair time and seek multiple medical opinions for the same symptoms. They are the people who tend to claim unresponsiveness to traditional therapies yet claim unique responsiveness to the side effects of these therapies. Often, these patients misinterpret reassurance as dismissiveness.
What happens if we combine the DEWS definition of DED with the DSM-5’s definition of SSD? Ultimately, we find a complex and diverse pathophysiology compounded by a complex and diverse psychology, wherein the way the patient perceives the disease influences how he or she experiences the disease. It is important to note, however, that the DSM-5 definition is new; in the previous version, the DSM-4, the emphasis was on medically unexplained symptoms. With the inclusion of SSD in the DSM-5, however, emphasis was directed toward the somatic origins of symptoms to diminish the suggestion that such symptoms existed “only in the head”—in other words, to de-emphasize the idea of a mind-body dualism.
THE MIND-BODY CONNECTION
For millennia, philosophers and scientists have grappled with the question of mind-body dualism. Can the mind exist separately from our physical bodies and brains? Certainly, modern physiology and neurobiology would not allow for this possibility. Increasingly, we have a firm grasp on the neurochemical and neuroelectrical underpinnings that explain our sentient, conscious state. Well-known philosophers such as the 17th-century philosopher Rene Descartes, however, argued emphatically for the separation of mind and body and believed the processes of the mind existed independently of the body.
Of course, Descartes did not have our knowledge of physiology. He never knew the direct physiologic effects the mind has on the body in the “fight-or-flight” response. He never knew the results of psychological stress on the cardiovascular system, the gastrointestinal system, and the immune system. He never knew the direct consequences that placebos have on physiologic processes. Furthermore, physicians commonly connect certain disease states to anxiety states, such as in fibromyalgia, chronic fatigue syndrome, and irritable bowel syndrome. Should we add DED to this list?
THE PSYCHOLOGY OF DED
At this point, one might argue that the interaction of the mind and body in disease states is so basic that it could be applied equally to any disease. That is true; however, DED is unique. This is because it has both a unique pathophysiology and a unique set of psychologies.
Its distinct pathophysiology derives from the fact that (1) most patients do not even recognize it as a disease, (2) the signs and symptoms do not correlate, (3) no universal lab or objective test for diagnosis exists, (4) there is enormous variability in its presentation, (5) multiple masquerading syndromes exist, and (6) many doctors do not fully understand the inflammatory basis of chronic DED.
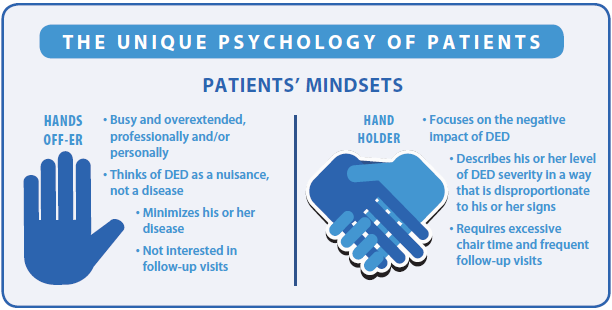
With regard to the unique psychologies of DED, our default is to think of DED patients solely in terms of the anxious, time-consuming variety, labeled “hand holders” in the figure. We must not forget, however, the equally important category of DED patients labeled “hands off-ers.” The latter category is typically the young, busy professional who dismisses DED as inconsequential, prefers to receive no treatment, and requests to return in 1 year.
By simply and rapidly identifying which patient type is in the examination chair, the doctor can find the right balance of care and attention that each patient type prefers without coming across as overbearing to the “hands-off-er” or underattentive to the “hand-holder.”
Physicians, too, suffer from our own unique psychologies when managing DED. We are frequently affected by three biases about DED: the ideas that treatment is (1) futile, (2) time-consuming, and (3) unprofitable. However, all three of these are wrong. With the proper blend of customization of treatment, innovation in diagnostics and devices, and improved practice organization, doctors can quickly align their DED program to be
(1) effective, (2) efficient, and (3) profitable.
TREATING MIND AND BODY
Many readers at this point may be satisfied that doctors need to improve their awareness of the psychology of DED. How should we go about incorporating this into daily practice? There are three simple steps: explain, objectify, and inspire. We must explain to patients that they actually have a disease—a disease that can get better or worse and for which treatment options are available. By our framing their symptoms within the concept of disease, patients will have a more realistic understanding of why they need treatment and what they should expect from their treatment.
DED has classically suffered from a paucity of objective tests. For this reason, the need to objectify carries unique importance. Unlike glaucoma patients who typically leave with a number representing their IOP, DED patients typically leave with nothing. With the advent of new diagnostics such as osmolarity testing and InflammaDry (Rapid Pathogen Screening), doctors have new ways to validate a patient’s progress (or lack thereof). These numbers can serve as “mile markers” for patients, giving them goals and improving compliance.
Finally, we need to inspire both our patients and ourselves. We now have an improved understanding of the inflammatory basis of chronic DED. We must remind ourselves that we have the chance to treat this inflammation earlier and to effect earlier improvement. We can also better manage our patients’ expectations, and, in doing so, we can inspire them and reduce disappointment. As our knowledge of T cells, cytokines, and interleukins increases, we must never forget about the importance of patients’ perception. We must never forget about the person behind the eyes. Once we admit that the mind and body do interact in disease, we must never forget what happens when the mind’s eye goes dry. n
1. Dry Eye Workshop. The definition and classification of dry eye disease: report of the definition and classification subcommittee of the International Dry Eye Workshop. Ocul Surf. 2007;5:75-92.
2. The Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, D.C.: American Psychiatric Association; 2013.
Richard A. Adler, MD
• director at Belecara Health Ophthalmology
• assistant professor of ophthalmology at Wilmer Eye Institute, Baltimore, Maryland
• dradler@belecara.com
• financial disclosure: consultant to Allergan


